100 questions match your search.
A 70-kg 58-year-old man with unstable angina is scheduled to undergo coronary artery bypass grafting. Intravenous heparin and nitroglycerin are administered for four days before surgery. Before initiating cardiopulmonary bypass, 21,000 units of heparin are administered through the central venous catheter; five minutes later, activated clotting time is 280 seconds. Which of the following is the most appropriate next step in management?
- (A) Discontinue nitroglycerin
- (B) Administer additional heparin
- (C) Administer cryoprecipitate
- (D) Administer fresh frozen plasma
- (E) Initiate cardiopulmonary bypass
Hemodilution is used during profound hypothermic cardiopulmonary bypass primarily because it
- (A) decreases cold-induced coagulopathy
- (B) decreases edema formation
- (C) increases oxygen-carrying capacity of plasma
- (D) increases oxygen dissociation from hemoglobin
- (E) limits the cold-induced increase in blood viscosity
Pulsus paradoxus is commonly seen during anesthesia in patients with each of the following conditions EXCEPT
- (A) severe asthma
- (B) right-sided heart failure
- (C) hypovolemia
- (D) atrial septal defect
- (E) obesity
You are called to anesthetize a patient for an emergency pericardial window for a large pericardial effusion. Which of the following drugs is most appropriate for initiation of anesthesia?
- (A) Alfentanil
- (B) Ketamine
- (C) Midazolam
- (D) Propofol
- (E) Thiopental
A 50-year-old man with severe coronary artery disease undergoes coronary artery bypass grafting. Five minutes after successful termination of cardiopulmonary bypass, ST-segment elevation is noted in lead II of the ECG, and the following findings are noted: BP 70/40, Pulse 80, CVP 16 cmH2O, PAp 25/10. Appropriate management is to
- (A) administer propranolol
- (B) administer nitroglycerin
- (C) administer dopamine
- (D) administer crystalloid fluid
- (E) return the patient to cardiopulmonary bypass
Which of the following pre-existing conditions predisposes to new-onset third-degree heart block during pulmonary artery catheterization?
- (A) First-degree heart block
- (B) Left bundle branch block
- (C) Sick sinus syndrome
- (D) Sinus bradycardia
- (E) Wenckebach second-degree heart block
During induction of anesthesia in a 70-year-old man with aortic stenosis, the blood pressure decreases from 140/ 80 to 70/45 mmHg as the cardiac rhythm changes from normal sinus at 70 bpm to junctional at 120 bpm. The most appropriate initial therapy would be
- (A) cardioversion
- (B) esmolol
- (C) fluid bolus
- (D) phenylephrine
- (E) verapamil
Which of the following statements concerning isolated mitral stenosis is true?
- (A) Afterload reduction increases cardiac output
- (B) Pulmonary artery occlusion pressure overestimates left ventricular filling pressure
- (C) Pulmonary hypertension is irreversible
- (D) Tachycardia decreases the mitral transvalvular gradient
- (E) Thermodilution cardiac output measurements are unreliable
The tracing indicates that the pacemaker generator is
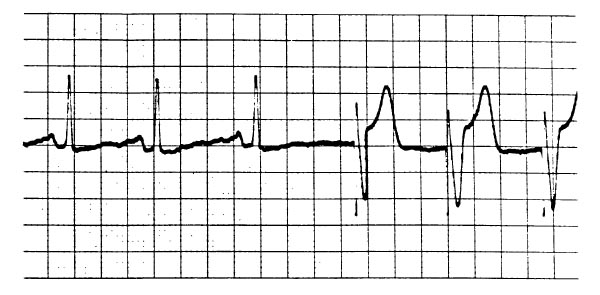
- (A) malfunctioning
- (B) VVT sensing and capturing normally
- (C) VOO sensing and capturing normally
- (D) DVI sensing and capturing normally
- (E) VVI sensing and capturing normally
Increasing preload, systemic vascular resistance and heart rate will best maintain hemodynamic stability in patients with
- (A) aortic stenosis
- (B) asymmetric septal hypertrophy (IHSS)
- (C) cardiac tamponade
- (D) mitral regurgitation
- (E) mitral stenosis
Left ventricular end-diastolic volume is most likely to be underestimated by pulmonary artery occlusion pressure in patients with
- (A) acute myocardial ischemia
- (B) aortic insufficiency
- (C) mitral stenosis
- (D) primary pulmonary hypertension
- (E) tricuspid stenosis
In the diagram, point "X" represents a patient with severe left ventricular dysfunction. The points labeled 1, 2, and 3 each represent the results of a different therapeutic intervention. Which of the following represents the most likely intervention at each point?
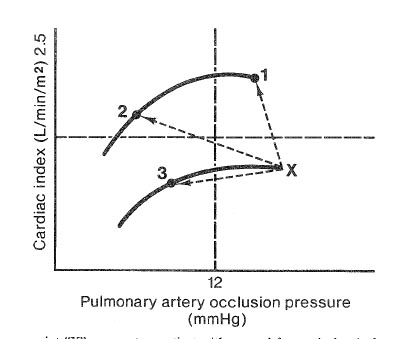
- (A) 1-Dopamine, 2-Furosemide, 3-Nitroprusside
- (B) 1-Dopamine, 2-Nitroprusside, 3-Furosemide
- (C) 1-Furosemide, 2-Dopamine, 3-Nitroprusside
- (D) 1-Nitroprusside, 2-Dopamine, 3-Furosemide
- (E) 1-Nitroprusside, 2-Furosemide, 3-Dopamine
Pulmonary artery diastolic pressure increases acutely from 10 to 20 mmHg in a 28-year-old man undergoing cervical laminectomy in the sitting position. The most appropriate first step in the management of this patient is to
- (A) administer furosemide
- (B) aspirate from the proximal port of the pulmonary artery catheter
- (C) inflate the balloon on the pulmonary artery catheter
- (D) place the patient in the left lateral decubitus position
- (E) start an infusion of nitroglycerin
Two hours after coronary artery bypass grafting, a 60-year-old man has a heart rate of 140 bpm and blood pressure of 80/60 mmHg. Cardiac index is 1.5 L/min/m2. Central venous pressure is 23 mmHg with large a-waves in the right atrial pressure tracing. A pulsus paradoxus of 6 mmHg is noted. Which of the following is the most likely diagnosis?
- (A) Atrial flutter
- (B) Cardiac tamponade
- (C) Hypovolemia
- (D) Junctional tachycardia
- (E) Tension pneumothorax
Which of the following is the best method of pacing to improve cardiac output in a patient with third-degree heart block?
- (A) VOO
- (B) AOO
- (C) VVI
- (D) DVI
- (E) Transcutaneous
After termination of cardiopulmonary bypass, a patient who is chronically digitalized receives digoxin 0.5 mg in error. An ECG shows sinus bradycardia with intermittent sinus arrest; blood pressure is 90/60 mmHg. Which of the following drugs is contraiindicated in this patient?
- (A) Atropine
- (B) Calcium chloride
- (C) Ephedrine
- (D) Magnesium sulfate
- (E) Phenylephrine
Which of the following is the most appropriate drug to treat hypotension in patients with asymmetric septal hypertrophy (IHSS)?
- (A) Amrinone
- (B) Calcium chloride
- (C) Dopamine
- (D) Ephedrine
- (E) Phenylephrine
A 55-kg, 70-year-old woman with mild chronic renal failure is unresponsive 20 hours after an uneventful coronary artery bypass grafting procedure. Anesthetic drugs included fentanyl 3000 mcg, diazepam 35 mg, and pancuronium 20 mg. Which of the following is the most appropriate next step in management?
- (A) Administration of edrophonium
- (B) Administration of flumazenil
- (C) Administration of naloxone
- (D) CT scan of the head
- (E) Measurement of core body temperature
Which of the following is the primary factor regulating normal coronary blood flow?
- (A) Aortic diastolic pressure
- (B) Coronary perfusion pressure
- (C) Heart rate
- (D) Myocardial oxygen consumption
- (E) Systolic wall tension
After weaning from cardiopulmonary bypass following mitral valve replacement, a patient's cardiac output is reported to be 3.7 L/min measured by thermodilution technique using 5% dextrose in water 10 ml at room temperature as injec-tate. This value could be falsely high if
- (A) normal saline solution were mistakenly used
- (B) the patient's hematocrit were still 25%
- (C) only 9.0 ml of injectate were used
- (D) atrial fibrillation were present
- (E) the room were excessively cold
During cardiopulmonary bypass at a nasopharyngeal temperature of 28°C and a hematocrit of 20%, temperature-corrected PaCO2 is 50 mmHg and uncorrected PaCO2 is 60 mmHg. The most appropriate management is to
- (A) administer additional opioid
- (B) administer packed red blood cells to increase hematocrit to 25%
- (C) further decrease the patient's temperature
- (D) increase fresh gas flow to the oxygenator
- (E) institute mechanical ventilation
A 65-year-old patient with hypertrophic cardiomyopathy has chest pain prior to induction of anesthesia. Pulse is 80 bpm and blood pressure is 130/80 mmHg. The ECG (V5) shows sinus rhythm and new ST-segment depression. The most appropriate management is administration of
- (A) furosemide
- (B) metoprolol
- (C) morphine
- (D) nifedipine
- (E) nitroglycerin
A patient receiving propranolol and nifedipine is scheduled for elective coronary artery bypass surgery. During induction with fentanyl and oxygen, heart rate decreases from 52 to 36 bpm and blood pressure decreases from 130/85 to 80/50 mmHg. Administration of atropine 2 mg intravenously has no effect. The most appropriate treatment at this time is administration of
- (A) epinephrine
- (B) pancuronium
- (C) naloxone
- (D) phenylephrine
- (E) calcium chloride
A 1100-g, 10-day-old infant is to undergo ligation of a patent ductus arteriosus after unsuccessful medical treatment. Within three minutes of intravenous administration of atropine 20 mcg, fentanyl 20 mcg, and pancuronium 0.1 mg, systemic blood pressure decreases from 80 to 30 mmHg, heart rate from 180 to 140 bpm, and arterial oxygen saturation from 90% to 80%. The most appropriate management is to
- (A) increase FiO2
- (B) administer additional atropine
- (C) infuse crystalloid
- (D) infuse prostaglandin E1
- (E) administer phenylephrine
Intraoperatively, the occurrence of prominent "a" waves on the central venous pressure waveform can be explained by each of the following EXCEPT
- (A) acute right ventricular failure
- (B) atrial flutter
- (C) complete heart block
- (D) onset of junctional tachycardia
- (E) ventricular pacing
Three hours after undergoing coronary artery bypass grafting, an elderly man develops severe hypotension after intravenous administration of morphine 4 mg. Pulmonary artery occlusion pressure is 27 mmHg and central venous pressure is 30 mmHg. Transesophageal echocardiography shows decreased end-diastolic ventricular volumes. Which of the following is the most likely diagnosis?
- (A) Anaphylactoid reaction
- (B) Cardiac tamponade
- (C) Coronary graft occlusion
- (D) Excessive fluid administration
- (E) Pulmonary thromboembolus
Compared with dopamine, dobutamine
- (A) is more useful in patients taking monoamine oxidase inhibitors because it depends on the release of norepinephrine for its effect
- (B) is more useful in patients in right heart failure because it does not increase pulmonary vascular resistance
- (C) has no positive chronotropic response
- (D) induces diuresis without increasing cardiac output
- (E) in doses greater than 10 mcg/kg/min increases systemic vascular resistance more than similar doses of dopamine
Which of the following effects of catecholamine results in the greatest increase in preload?
- (A) Augmented contractility
- (B) Decreased afterload
- (C) Decreased venous capacitance
- (D) Improved chronotropism
- (E) Increased cardiac output
During uncomplicated mask induction with halothane and 50% nitrous oxide in oxygen in a 6-month-old infant with a large ventricular septal defect and valvular pulmonic stenosis, SpO2 decreases from 85% (room air) to 60%; heart rate is 100 bpm and blood pressure is 62/40 mmHg. The most appropriate management is to
- (A) administer atropine
- (B) administer phenylephrine
- (C) administer propranolol
- (D) increase anesthetic depth
- (E) intubate the trachea
Four days after mitral valve replacement, a 49-year-old, 70-kg woman who has had oliguric renal failure since the operation requires insertion of a Schribner shunt for hemodialysis. Her BUN concentration is 104 mg/dl, serum creatinine is 9.3 mg/dl, serum sodium is 130 mEq/L, and serum potassium is 6.7 mEq/L. During the operation under local anesthesia, diazepam 7.5 mg and morphine 10 mg are administered intravenously to control agitation. Five minutes later while she is sleeping quietly, unifocal premature ventricular contractions appear at a rate of 10 per minute on the ECG monitor. The most appropriate therapy is to
- (A) administer calcium gluconate 250 mg intravenously
- (B) augment ventilation with bag and mask
- (C) administer lidocaine 100 mg intravenously
- (D) administer NaHC03 50 mEq intravenously
- (E) observe only
A 62-year-old man is undergoing elective coronary artery bypass grafting and aortic valve replacement for three-vessel coronary artery disease and aortic stenosis. Shortly after intubation, heart rate increases from 75 to 100 bpm and blood pressure decreases from 130/70 to 70/40 mmHg with acute, severe ST-segment depression in lead V5. Which of the following is the most appropriate management?
- (A) Crystalloid
- (B) Ephedrine
- (C) Esmolol
- (D) Nitroglycerin
- (E) Phenylephrine
Following blunt trauma to the chest, a patient has tachycardia, hypotension, and markedly distended neck veins. Each of the following is expected EXCEPT
- (A) cardiac output of 2.1 L/min
- (B) mixed venous oxygen saturation of 75%
- (C) pulmonary artery occlusion pressure of 25 mmHg
- (D) pulmonary artery diastolic pressure of 25 mmHg
- (E) right atrial pressure of 25 mmHg
A 14-month-old child has tetralogy of Fallot with dynamic obstruction to right ventricular outflow. Which of the following is most likely to decrease cyanosis in this child?
- (A) Calcium
- (B) Epinephrine
- (C) Nitroglycerin
- (D) Nitroprusside
- (E) Propranolol
A 5-month-old infant with tetralogy of Fallot is scheduled for elective inguinal herniorrhaphy. Which of the following would require the operation to be postponed?
- (A) Current propranolol therapy
- (B) Hematocrit of 65%
- (C) History of "tet spells"
- (D) Patent ductus arteriosus
- (E) Room air oxygen saturation of 82%
Spinal anesthesia at a T6 sensory level is most likely to improve cardiac output in patients with
- (A) aortic stenosis
- (B) asymmetric septal hypertrophy (IHSS)
- (C) chronic constrictive pericarditis
- (D) cor pulmonale
- (E) mitral regurgitation
Addition of 20 cm H2O positive end-expiratory pressure to a patient receiving controlled mechanical ventilation decreases cardiac output and left ventricular function by
- (A) increasing right ventricular preload
- (B) increasing right ventricular afterload
- (C) increasing left ventricular preload
- (D) increasing left ventricular afterload
- (E) producing myocardial ischemia
An arterial blood sample is obtained from a patient undergoing hypothermic cardiopulmonary bypass at 28 C. Analysis at 37 C shows a pH of 7.40 and PaCO2 of 40 mmHg. Which of the following values are most likely if the analysis is corrected to 28 C?
- (A) pH = 7.40; PaCO2 = 40
- (B) pH > 7.40; PaCO2 < 40
- (C) pH > 7.40; PaCO2 > 40
- (D) pH < 7.40; PaCO2 < 40
- (E) pH < 7.40; PaCO2 > 40
A 65-kg, 57-year-old man has an initial activated clotting time (ACT) of 122 seconds prior to elective cardiopulmonary bypass. Five minutes after administration of heparin 200 mg, ACT increases to 154 seconds. After two additional doses of 200 mg each from different lots, ACT increases to 240 seconds. The most appropriate next step is to
- (A) administer additional heparin 400 mg
- (B) administer fresh frozen plasma 2 units
- (C) initiate cardiopulmonary bypass
- (D) measure the plasma heparin concentration
- (E) start an infusion of desmopressin
Hypomagnesemia is associated with
- (A) decreased risk for digitalis toxicity
- (B) dysrhythmias sensitive to bretylium
- (C) hypercalcemia
- (D) prolonged succinylcholine blockade
- (E) surgery requiring cardiopulmonary bypass
An atrioventricular sequential demand pacemaker is placed in a patient who has abnormal atrioventricular conduction. Each of the following statements about this situation is true EXCEPT:
- (A) Electrocautery could lead to long pauses in the paced rhythm
- (B) Placing a magnet over the generator will convert it to an asynchronous (fixed rate) unit
- (C) If complete heart block develops, the paced ventricular rate will be the same as the sinus node rate
- (D) An atropine-induced increase in the sinus rate will increase the ventricular rate
- (E) During symptomatic tachyarrhythmia, cardioversion would be contraindicated because it would alter the pacemaker's function
A 67-kg, 52-year-old man is undergoing heart transplantation. After implantation of the donor heart and discontinuation of cardiopulmonary bypass, isoproterenol is administered intravenously to maintain heart rate greater than 100 bpm. During the next 10 minutes, blood pressure decreases from 105/55 mmHg to 75/40 mmHg. Heart rate is 102 bpm and cardiac output is 5.8 L/min. The most appropriate management is administration of
- (A) amrinone
- (B) digoxin
- (C) dopamine
- (D) epinephrine
- (E) norepinephrine
An adult patient with atrial fibrillation develops pulseless ventricular tachycardia wfiile undergoing synchronized electirical cardioversion. Which of the following is the most appropriate management?
- (A) Intravenous administration of adenosine
- (B) Intravenous administration of a bolus of lidocaine followed by electrical cardioversion
- (C) Immediate repeat synchronized cardioversion at the same energy level
- (D) Immediate repeat synchronized cardioversion at twice the previous energy level
- (E) Unsynchronized electrical cardioversion
A 46-year-old patient who abuses intravenous drugs develops acute aortic valvular insufficiency from bacterial endocarditis. Which of the following statements concerning pressures measured through a pulmonary artery catheter is true?
- (A) Pulmonary artery occlusion pressure will underestimate left ventricular end-diastolic pressure
- (B) Pulmonary artery oxygen saturation will overestimate mixed venous oxygen saturation
- (C) Thermodilution cardiac output determination will overestimate cardiac output
- (D) Right ventricular end-diastolic pressure will equal left ventricular end-diastolic pressure
- (E) The pulmonary artery occlusion pressure trace will most likely have large V waves
Which of the following is the most likely cause of the coronary steal phenomenon?
- (A) Idiopathic hypertrophic subaortic stenosis (IHSS)
- (B) Decreased cardiac contractility
- (C) Dilation of coronary arterioles
- (D) Dilation of epicardial coronary arteries
- (E) Increased systemic vascular resistance
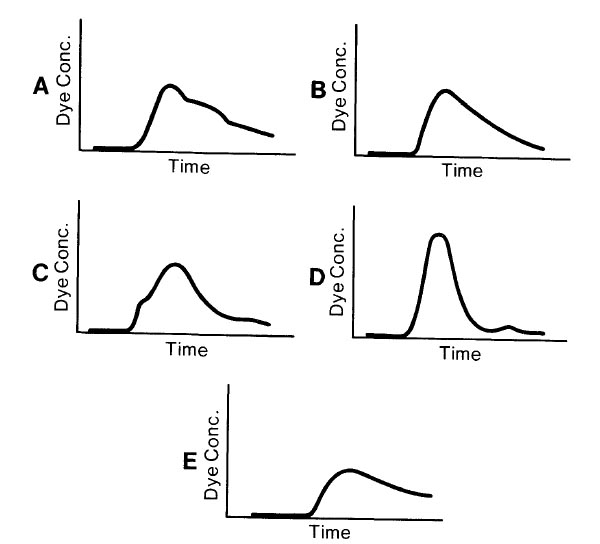
Which of the following time concentration curves would be expected in arterial blood following intravenous injection of indocyanine green dye in a 3-year-old child with a small ventricular septal defect?
Which of the following is the most appropriate management of decreased cardiac output in patients with isolated aortic insufficiency?
- (A) Dobutamine
- (B) Esmolol
- (C) Intra-aortic balloon counterpulsation
- (D) Norepinephrine
- (E) Positive pressure ventilation
Which of the following results in the greatest increase in right-to-left shunting in an infant with cyanotic heart disease?
- (A) Decreased pulmonary vascular resistance
- (B) Decreased systemic vascular resistance
- (C) Hemodilution
- (D) Increased heart rate
- (E) Myocardial depression
The tracing indicates that the pacemaker generator is
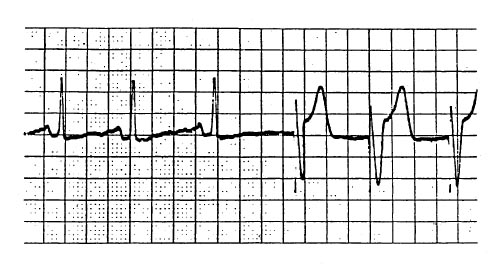
- (A) malfunctioning
- (B) VVT sensing and capturing normally
- (C) VOO sensing and capturing normally
- (D) DVI sensing and capturing normally
- (E) VVI sensing and capturing normally
Following cardiopulmonary bypass, right ventricular distention is noted after infusion of protamine 40 mg. Pulmonary artery pressure has increased from 25/18 to 50/30 mmHg and systemic arterial pressure has decreased from 110/65 to 0 mmHg. Which of the following is the most appropriate treatment?
- (A) Administration of amrinone
- (B) Administration of nitroglycerin
- (C) Administration of phenylephrine
- (D) Initiation of intra-aortic balloon pump assist
- (E) Reheparinization and resumption of cardiopulmonary bypass
An 18-month-old child with tetralogy of Fallot is anesthetized with halothane and nitrous oxide. Following intubation, oxygen saturation decreases abruptly from 85% to 45%. The most effective treatment is
- (A) discontinuation of halothane
- (B) hyperventilation
- (C) intravenous epinephrine
- (D) intravenous phenylephrine
- (E) positive end-expiratory pressure
Addition of 20 cmH2O positive end-expiratory pressure to a patient receiving controlled mechanical ventilation decreases cardiac output and left ventricular function by
- (A) increasing right ventricular preload
- (B) increasing right ventricular afterload
- (C) increasing left ventricular preload
- (D) increasing left ventricular afterload
- (E) producing myocardial ischemia
A 35-year-old patient with asymmetric septal hypertrophy (IHSS) is undergoing bladder suspension with sevoflurane 1%, nitrous oxide 50%, and oxygen 50%. Immediately after skin incision, blood pressure decreases to 90/60 mmHg and junctional tachycardia of 150 bpm is noted on the ECG. Which of the following is the most appropriate management?
- (A) Decreasing sevoflurane concentration
- (B) Infusion of nitroglycerin
- (C) Intravenous administration of a fluid bolus
- (D) Intravenous administration of esmolol
- (E) Intravenous administration of phenylephrine
In a patient with ventricular fibrillation refractory to repeated attempts at defibrillation and epinephrine administration, the most appropriate management is administration of
- (A) amiodarone
- (B) procainamide
- (C) propranolol
- (D) quinidine
- (E) verapamil
A 70-kg, 47-year-old man is undergoing a repeat coronary artery bypass graft. Following sternotomy, administration of heparin 300 units/kg for anticoagulation increases the activated coagulation time from a baseline of 135 sec to 210 sec. This finding is compatible with
- (A) antithrombin III deficiency
- (B) heparin-induced thrombocytopenia
- (C) normal response to this dose of heparin
- (D) increased sensitivity to heparin
- (E) von Willebrand's disease
During protamine administration following separation from cardiopulmonary bypass, blood pressure decreases from 100/70 to 60/30 mmHg and peak inspiratory pressure increases from 26 to 60 cm H2O. The most appropriate next step in management is administration of
- (A) diphenhydramine
- (B) dopamine
- (C) epinephrine
- (D) methylprednisolone
- (E) terbutaline
The ECG strip shown is recorded as a patient with a permanent transvenous DDD pacemaker enters the operating room. These changes indicate that the pacemaker is
- (A) sensing the T waves
- (B) sensing the retrograde P waves
- (C) triggering off the intrinsic atrial activity
- (D) malfunctioning in the atrial pacing mechanism
- (E) prematurely stimulating the ventricle
A 70-year-old patient is shivering and has chest pain in the PACU following a cholecystectomy. Heart rate is 120 bpm, and blood pressure is 220/120 mmHg. SpO2 is 97% at an FiO2 of 0.4. An ECG shows ST-T wave changes, which are not affected by intravenous administration of nitroglycerin. Which of the following is the most appropriate next step?
- (A) Administration of esmolol
- (B) Administration of hydralazine
- (C) Administration of nitroprusside
- (D) Application of a warming blanket
- (E) Increasing FiO2
A 68-year-old man has a permanent DVI pacemaker that has been functioning appropriately. Which of the following is most likely to cause conversion to VOO pacing?
- (A) Electroconvulsive therapy
- (B) Insertion of a pulmonary artery catheter
- (C) Placement of a magnet over the pulse generator
- (D) Use of electrocautery near the pacemaker
- (E) Shivering
A 62-year-old man, who had a myocardial infarction three years ago, complicated by congestive heart failure and renal failure, is undergoing a colectomy. A pulmonary artery catheter demonstrates a cardiac output higher than measurements recorded during a cardiac catheterization two months after the infarction. Which of the following most likely contributes to the increased cardiac output?
- (A) Creation of an arteriovenous fistula
- (B) Increased hemoglobin concentration from 10 to 12 g/dl
- (C) Stimulation of carotid body receptors
- (D) Transcutaneous nitroglycerin
- (E) Use of a beta-adrenergic blocker to prevent myocardial reinfarction
Which of the following findings is most likely in patients receiving intravenous milrinone?
- (A) Decreased left ventricular afterload
- (B) Decreased myocardial oxygen consumption
- (C) Increased atrioventricular conduction
- (D) Increased right ventricular preload
- (E) Stimulation of beta-adrenergic receptors
Nitroprusside therapy for hypertension should be discontinued in the presence of
- (A) acute myocardial infarction
- (B) increasing metabolic acidosis
- (C) methemoglobinemia
- (D) mitral regurgitation
- (E) renal failure
Left ventricular end-diastolic volume is most likely to be underestimated by pulmonary artery occlusion pressure in patients with
- (A) acute myocardial ischemia
- (B) aortic insufficiency
- (C) mitral stenosis
- (D) primary pulmonary hypertension
- (E) tricuspid stenosis
As part of a preoperative evaluation, a patient had a thallium scan showing a "cold spot" over the left ventricle that occurs with moderate exercise and disappears at rest. This most likely indicates
- (A) moderate-sized aneurysm of the left ventricle
- (B) acute myocardial ischemia
- (C) recent myocardial infarction
- (D) old myocardial infarction
- (E) Prinzmetal's variant angina
A patient who is receiving ventilatory support after coronary artery bypass grafting has a PaO2 of 132 mmHg, a PaCO2 of 19 mmHg, and a pH of 7.57. Which of the following is most likely to result from this level of hypocarbia?
- (A) Decreased airway resistance
- (B) Increased myocardial contractility
- (C) Hyperkalemia
- (D) Shortened QT interval
- (E) Cerebral ischemia
During cardiopulmonary bypass, the perfusionist notes that the mixed venous oxygen saturation has decreased from to 55%. Which of the following is the most likely cause?
- (A) Administration of a nitroprusside bolus
- (B) Administration of a thiopental bolus
- (C) Decrease in rectal temperature from 34°C to 28°C
- (D) Inadequate muscle relaxation
- (E) Increase in pump flow
During repair for coarctation of the aorta in a healthy 13-year-old patient, right radial artery pressure increases from 100/60 to 105/70 mmHg after the aorta is cross clamped. This most likely indicates that
- (A) collateral blood flow has decreased the hemodynamic consequences of cross-clamping
- (B) left ventricular hypertrophy has decreased left ventricular compliance
- (C) spinal cord blood flow is impaired
- (D) the coarctation has decreased aortic diameter less than 50%
- (E) the coarctation involves the origin of the right subclavian artery
In patients who have undergone cardiopulmonary bypass, administration of milrinone is most likely to result in an increase in which of the following?
- (A) Arterial blood pressure
- (B) Heart rate
- (C) Pulmonary capillary wedge pressure
- (D) Stroke volume
- (E) Systemic vascular resistance
Which of the following is most likely to result in oxygen desaturation in a patient with Eisenmenger's syndrome who is scheduled for cesarean delivery?
- (A) Breathing room air
- (B) Epidural administration of lidocaine
- (C) Intravenous administration of ketamine
- (D) Intravenous administration of ephedrine
- (E) Mild hypocarbia
A 66-year-old man with aortic regurgitation is brought to the operating room for aortic valve replacement after having received morphine, scopolamine premedication. PO2 is 40 mmHg in a sample of pulmonary artery blood drawn 10 minutes after the patient started breathing pure oxygen. This finding is compatible with
- (A) wedging of the catheter tip
- (B) left-to-right intracardiac shunt
- (C) increased intrapulmonary shunting
- (D) excessively depressed ventilation
- (E) normal cardiac output
A 69-year-old woman with mitral stenosis and atrial fibrillation is scheduled for mitral valve replacement and removal of a left atrial thrombus. After administration of pancuronium, heart rate increases to 140 bpm and blood pressure decreases to 70/40 mmHg. Which of the following is the LEAST appropriate treatment?
- (A) Cardioversion
- (B) Edrophonium
- (C) Esmolol
- (D) Phenylephrine
- (E) Verapamil
An EKG shows ventricular tachycardia in a patient with a heart rate of 160 bpm and a blood pressure of 90/60 mmHg. The best initial therapeutic maneuver prior to cardioversion is
- (A) carotid sinus massage
- (B) intravenous administration of bretylium
- (C) intravenous administration of amiodarone
- (D) intravenous administration of propranolol
- (E) precordial "thump"
As part of a preoperative evaluation, a patient had a thallium scan showing a 'cold spot' over the left ventricle that occurs with moderate exercise and disappears at rest. This most likely indicates
- (A) moderate-sized aneurysm of the left ventricle
- (B) acute myocardial ischemia
- (C) recent myocardial infarction
- (D) old myocardial infarction
- (E) Prinzmetal's variant angina
The following hemodynamic values are obtained two hours after coronary artery bypass surgery: Cardiac index 1.7 L/min/m2; Pulm Art. Occ. Pressure 22 mmHg; MAP 60 mmHg; Urine volume 0.2 ml/kg/hr. The most appropriate management is
- (A) dopamine infusion
- (B) nitroprusside infusion
- (C) norepinephrine infusion
- (D) volume expansion
- (E) observation without intervention
Following hypothermic cardiopulmonary bypass, adequacy of total body rewarming is best indicated by normothermia recorded from the
- (A) upper esophagus
- (B) lower esophagus
- (C) pulmonary artery
- (D) rectum
- (E) great toe
In the absence of coronary artery disease, isoflurane-induced vasodilation and tachycardia are beneficial hemodynamic goals for which of the following cardiac diseases?
- (A) Aortic regurgitation
- (B) Aortic stenosis
- (C) Asymmetric septal hypertrophy (IHSS)
- (D) Mitral stenosis
- (E) Pulmonary regurgitation
A 67-year-old man is undergoing total hip replacement under general anesthesia. He had a permanent endocardial VVI pacemaker placed two years ago for complete heart block, and since arrival in the operating room has been paced continuously. Use of the electrocautery causes the pacemaker to malfunction intermittently. The most appropriate management is to
- (A) tape a magnet over the pacemaker generator and convert to asynchronous mode
- (B) do nothing since the pacemaker is programmed to deal with this circumstance
- (C) stop the surgeon from using the electrocautery
- (D) limit the surgeon to 10 sec/min electrocautery bursts
- (E) place the electrocautery indifferent lead as close as possible to the pacemaker
A 55-year-old man who is scheduled to undergo carotid endarterectomy (CEA) has a persistent myocardial filling defect at three hours on a dipyridamole-thallium scan. Which of the following statements is correct?
- (A) Coronary autoregulation is effective in this segment
- (B) Coronary revascularization should precede CEA
- (C) Isoflurane is contraindicated
- (D) Myocardial infarction is impending
- (E) There is a segment of nonviable myocardium
Each of the following conditions can be accurately evaluated with transesophageal echocardiography EXCEPT
- (A) intimal tear at the aortic arch
- (B) intracardiac air
- (C) left atrial thrombus
- (D) patent foramen ovale
- (E) right atrial myxoma
A 45-year-old man is scheduled for appendectomy under general anesthesia. He reports that for many years he has occasionally felt his heart "skip a beat." The ECG tracing shown was obtained one hour ago. Which of the following is the most appropriate next step?
- (A) Proceeding with induction of anesthesia
- (B) Administration of a loading dose of digoxin
- (C) Carotid sinus massage
- (D) Intravenous administration of atropine
- (E) Placement of a temporary pacemaker
If a patient with excessive bleeding during exploratory laparotomy has a normal activated clotting time, the LEAST likely cause of the bleeding is
- (A) antithrombin III deficiency
- (B) dilutional thrombocytopenia
- (C) fibrinolysis
- (D) administration of heparin 5000 units
- (E) preoperative ingestion of aspirin
Following protamine administration, profound pulmonary hypertension is most likely initiated by release of
- (A) epinephrine
- (B) histamine
- (C) leukotriene
- (D) norepinephrine
- (E) thromboxane
Which of the following statements concerning use of temperature-corrected blood gas measurement (pH-stat) during hypothermic cardiopulmonary bypass is true?
- (A) Blood gas analysis is performed at the patient's temperature
- (B) Carbon dioxide should not be added to the bypass circuit
- (C) The carbon dioxide content of the patient's blood is greater than it would be without temperature correction
- (D) The incidence of postoperative neurologic deficits is increased compared with the alpha-stat method
- (E) The patient's temperature should be maintained above 25°C
A 75-year-old man with a left bundle branch block is undergoing placement of a pulmonary artery catheter through the right internal jugular vein. He becomes pale and his heart rate decreases to 40 bpm when the catheter tip enters the right ventricle. The most likely cause is
- (A) a catheter loop in the right atrium
- (B) acute myocardial infarction
- (C) acute pneumothorax
- (D) carotid sinus reflex
- (E) complete heart block
Each of the following is a physiologic effect of intra-aortic balloon pump therapy EXCEPT
- (A) decreased peak systolic pressure
- (B) increased cardiac output
- (C) increased coronary perfusion
- (D) increased diastolic pressure
- (E) increased total peripheral resistance
Pulmonary artery occlusion pressure
- (A) does not reliably reflect left ventricular end-diastolic volume when left ventricular compliance is reduced
- (B) inaccurately reflects left atrial pressure when left atrial pressure exceeds 15 mmHg
- (C) is measured at end-inspiration in mechanically ventilated patients
- (D) overestimates left atrial pressure in patients with poor lung compliance
- (E) reflects left atrial pressure only if the catheter tip is located in zone II of the lung
Cardiac output measured by thermodilution with a pulmonary artery catheter most accurately reflects systemic blood flow in a patient with
- (A) aortic regurgitation
- (B) atrial septal defect
- (C) patent ductus arteriosus
- (D) tricuspid insufficiency
- (E) ventricular septal defect
A 33-year-old woman is scheduled for emergency appendectomy under general anesthesia. She has hypertrophic cardiomyopathy and has had two episodes of syncope in the past year. Which of the following statements concerning anesthetic management is true?
- (A) Spinal anesthesia is preferred to general anesthesia
- (B) Deep levels of isoflurane anesthesia are appropriate
- (C) Fluid administration should be restricted
- (D) Phenylephrine is preferred to ephedrine to treat hypotension
- (E) Positive end-expiratory pressure will decrease left ventricular outflow obstruction
Which of the following findings necessitates the preoperative insertion of a ventricular pacemaker in a 48-year-old man scheduled to undergo cholecystectomy?
- (A) Atrial flutter with 3:1 atrioventricular block
- (B) Bifascicular (right bundle branch block and left anterior hemiblock) block
- (C) Left bundle branch block with first-degree atrioventricular block
- (D) Second-degree (Mobitz I) atrioventricular block
- (E) Second-degree (Mobitz II) atrioventricular block
Each of the following changes is expected with deliberate hypothermia EXCEPT
- (A) decreased unloading of oxygen from hemoglobin
- (B) a 5% decrease in MAC for each 1°C decrease in temperature
- (C) increased arterial oxygen and carbon dioxide contents
- (D) a 50% decrease in cerebral metabolic rate at 28°C
- (E) spike and dome EEG activity at temperatures below 30°C
A 32-year-old man is scheduled for hernia repair. He underwent heart transplantation for cardiomyopathy five years ago. Which of the following findings is most likely?
- (A) Absence of coronary atherosclerosis
- (B) Biventricular hypokinesis on echocardiography
- (C) Down-regulation of cardiac beta-adrenergic receptors
- (D) Increased heart rate at rest
- (E) Right ventricular hypertrophy
Which of the following findings would be considered normal in the EEG of an adult?
- (A) Decreased frequency during induction with halogenated anesthetics
- (B) Decreased frequency in frontal areas with administration of nitrous oxide 50%
- (C) Dominance of beta rhythm at 20 to 30 Hz during the awake relaxed state
- (D) Electrical silence with administration of isoflurane 2.5 MAC
- (E) The presence of burst-suppression during natural sleep
A patient has a heart rate of 110 bpm one year after heart transplantation. His tachycardia is most likely the result of
- (A) altered baroreceptor sensitivity
- (B) cardiac denervation
- (C) compensation for a fixed stroke volume
- (D) cyclosporine
- (E) prednisone
A 63-year-old man with a history of congestive heart failure and left ventricular dilation is scheduled for carotid endarterectomy. During carotid cross-clamping, the surgeon requests that systolic blood pressure be increased from 100 to 160 mmHg. Compared with an identical patient with normal left ventricular size, what is the effect of this change in blood pressure on this patient's myocardial oxygen consumption?
- (A) Equal decrease
- (B) Greater decrease
- (C) Lesser increase
- (D) Equal increase
- (E) Greater increase
Physiologically, coronary blood flow relates most directly to
- (A) cardiac work
- (B) systolic blood pressure
- (C) myocardial oxygen consumption
- (D) heart rate
- (E) mean arterial pressure
Which of the following best describes cardiomyopathy following therapy with doxorubicin (Adriamycin)?
- (A) The initial presentation is concentric hypertrophy
- (B) The diagnosis is confirmed by a shortened QT interval
- (C) It is exacerbated by hyperoxia
- (D) It is resistant to inotropic agents
- (E) It: may persist for years after therapy is discontinued
Each of the following statements concerning the activated clotting time (ACT) is true EXCEPT:
- (A) The ACT is more sensitive than the activated partial thromboplastin time (APTT) to blood heparin concentration
- (B) The ACT is prolonged if the specimen is not warmed during the assay
- (C) The ACT should be greater than 300 sec before initiating cardiopulmonary bypass
- (D) Hypofibrinogenemia may prolong the ACT after cardiopulmonary bypass
- (E) Whole blood is used for measurement of the ACT
In a patient with surgically significant aortic insufficiency, cardiac output measured by thermodilution will
- (A) be greater than right ventricular output
- (B) be less than left ventricular output
- (C) be less than cardiac output measured by the Fick method
- (D) be inaccurate because of decreased signal-to-noise ratio
- (E) underestimate net systemic arterial blood flow
Pulmonary artery diastolic pressure is an unreliable indicator of left ventricular end-diastolic pressure in patients with
- (A) acute cardiogenic pulmonary edema
- (B) aortic stenosis
- (C) acute mitral regurgitation
- (D) myocardial ischemia
- (E) severe emphysema
During total cardiopulmonary bypass, metabolic acidosis and decreasing mixed venous oxygen saturation are noted. The most likely cause is
- (A) hypothermia
- (B) hypoperfusion
- (C) hypocarbia
- (D) rewarming
- (E) light anesthesia
A 60-year-old obese man who has an antithrombin III deficiency is scheduled for radical prostatectomy. Prior to the operation this patient should receive
- (A) fresh frozen plasma
- (B) vitamin K
- (C) epsilon-aminocaproic acid
- (D) heparin
- (E) none of the above