135 questions match your search.
In a 5-kg child, the end-tidal carbon dioxide tension is 35 mmHg during spontaneous ventilation through a Mapleson D system. Which single change is most likely to increase this value?
- (A) Decreasing the fresh gas flow
- (B) Increasing respiratory minute volume
- (C) Opening the pressure release valve
- (D) Removing the reservoir bag
- (E) Substituting larger bore tubing
A neurologically intact 48-year-old woman is scheduled for removal of a parietal lobe arteriovenous malformation. The relative risk for complete resection is to be determined by a test occlusion of the feeding artery. Which of the following intraoperative monitoring techniques is most appropriate for this test?
- (A) Brain stem auditory evoked potentials
- (B) Cerebral blood flow using radioactive xenon
- (C) EEG
- (D) Evoked potentials elicited by stimulating the posterior tibial nerve
- (E) Transcranial Doppler
Which of the following decreases the risk for burns during electrocauterization?
- (A) Conductive flooring
- (B) Grounding of the patient to the operating table
- (C) Increased resistance at the return electrode
- (D) Isolation of the current output of the electrosurgical unit
- (E) Placement of the return electrode at a distance from the surgical site
Pulse oximetry accurately reflects SaO2 in which of the following situations?
- (A) Administration of indocyanine green
- (B) Administration of methylene blue
- (C) Carboxyhemoglobinemia
- (D) 40% fetal hemoglobin concentration
- (E) Methemoglobinemia
If the low-pressure alarm of an anesthesia circuit is broken, which of the following monitors will provide the earliest indication of a disconnected ventilator hose?
- (A) Fail-safe system
- (B) Infrared capnograph
- (C) Nitrogen analyzer
- (D) Oxygen analyzer
- (E) Pulse oximeter
Arterial pressure in the radial artery is 155/70 mmHg measured by a correctly calibrated catheter-transducer system. At the same time, aortic pressure is 140/75 mmHg using a high-fidelity catheter tip transducer. The most likely cause of this discrepancy is
- (A) a large amount of air in the dome of the radial artery transducer
- (B) coarctation of the aorta
- (c) peripheral vascular constriction produced by sympathetic stimulation
- (D) physiologic amplification of the waveform from the aorta to the radial artery
- (E) too high a frequency response in the catheter-transducer system
Which of the following malfunctions causes the line isolation monitor to alarm?
- (A) Discharge of static electricity
- (B) Flow of current to ground in the isolated circuit
- (C) Interruption of current to electrical outlets caused by a circuit breaker
- (D) Surge of current in the main power supply
- (E) Total electrical current exceeding circuit capacity
Which of the following is a characteristic of the Bain breathing circuit?
- (A) Condensation of moisture in inspired gases is facilitated by the circuit design
- (B) Fresh gas flows coaxially around the exhalation limb
- (C) Fresh gas flows need not exceed minute ventilation
- (D) The circuit eliminates the possibility of rebreathing
- (E) The circuit is functionally similar to the Jackson-Rees system
The most sensitive means of detecting venous air embolism is
- (A) precordial Doppler stethoscope
- (B) transesophageal echocardiography
- (C) end-tidal carbon dioxide measurement
- (D) pulmonary artery pressure measurement
- (E) central venous pressure measurement
After the bronchial and tracheal cuffs of a right endobronchial tube are inflated, ventilation through the tracheal lumen is not possible. This finding is most consistent with
- (A) cuff occlusion of the right upper lobe bronchus
- (B) intubation of the left bronchus
- (C) left-sided tension pneumothorax
- (D) overinflation of the bronchial cuff
- (E) positioning of both cuffs in the trachea
The risk for airway fire during laser resection of a tracheal tumor is decreased by use of
- (A) a CO2 laser rather than a YAG laser
- (B) an inspired helium concentration greater than 60%
- (C) an inspired nitrous oxide concentration greater than 60%
- (D) a polyvinylchloride endotracheal tube
- (E) halothane in the inspired mixture
Electrocautery units operate at frequencies between 300 kHz and 2 mHz to
- (A) avoid pacemaker interference
- (B) minimize ECG tracing interference
- (C) minimize the likelihood of ventricular fibrillation
- (D) optimize hemostasis
- (E) provide the best "cutting" current
A multi-orifices right heart catheter is being positioned by EKG control prior to sitting craniotomy. The EKG tracing is obtained between the distal tip of the catheter and the right arm lead. The most appropriate next step is to
- (A) leave the catheter in place
- (B) advance the catheter 2 to 3 cm
- (C) withdraw the catheter 2 to 3 cm
- (D) remove the catheter completely
- (E) change polarity of the EKG
Equipment that is attached to a patient should have leakage current no greater than
- (A) 10 microamps
- (B) 100 microamps
- (C) 1 milliamp
- (D) 10 milliamps
- (E) 100 milliamps
Which of the following is indicated by an alarm condition in the line-isolation monitor?
- (A) An electrical shock to the patient
- (B) A power surge in the main hospital power supply
- (C) Disconnection of the patient from an electrocautery grounding pad
- (D) Overload of the operating room circuits
- (E) The presence of a current leak between an operating room electrical device and ground
With respect to mechanical ventilation, which of the following statements concerning the portion of tidal volume known as compression volume is true?
- (A) It is calculated by dividing the volume of gas delivered to the patient by the peak pressure
- (B) It does not contribute to the volume of gas entering the patient
- (C) It is not included in the volume measured by a spirometer on the inspiratory limb
- (D) It decreases with the addition of a humidifier to the breathing circuit
- (E) It decreases with the addition of one-way valves at the Y connector of the breathing circuit
A 30-year-old man who is undergoing laparotomy and resection of a large kidney tumor has a decrease in SpO2 from 100% to 92% and an increase in peak airway pressure from 20 to 35 cm H2O. Plateau pressure is unchanged at 18 cm H2O. Which of the following is the most likely cause?
- (A) Abdominal packing
- (B) Inadequate anesthesia
- (C) Inadequate muscle relaxation
- (D) Obstruction of the endotracheal tube
- (E) Pneumothorax
The fail-safe mechanism on an anesthesia machine is activated by
- (A) a wall-oxygen pressure of less than 25 psi
- (B) a disconnection between the endotracheal tube and the machine
- (C) a nitrous oxide concentration in excess of 85%
- (D) an incompetent expiratory valve
- (E) no oxygen flow
A healthy, 18-year-old, 65-kg woman undergoing diagnostic laparoscopy is being monitored with a properly functioning and calibrated capnograph. The end-tidal carbon dioxide concentration is 6%, and the inspired carbon dioxide concentration is 1%. This may be caused by each of the following EXCEPT
- (A) malfunction of the expiratory valve in a circle system
- (B) low gas inflow with a Bain circuit
- (C) exhausted soda lime within a circle system
- (D) absorption of carbon dioxide from carbon dioxide laparoscopy
- (E) carbon dioxide in the fresh gas flow
A 27-month-old, 14-kg infant with intestinal obstruction is anesthetized with nitrous oxide at 1 L/min, oxygen at 0.4 L/min, and halothane at 0.8% using a Bain circuit. Ventilation is controlled at a rate of 30/min. The child's temperature is 39°C, and the PaCO2 is 65 mmHg. Which of the following is most likely?
- (A) Malignant hyperthermia
- (B) Low gas inflow rate
- (C) Low respiratory rate
- (D) Pulmonary aspiration of gastric contents
- (E) Inaccurate flowmeters
Which of the following is the most important function of temperature compensation in anesthetic vaporizers?
- (A) Compensation for changes in the specific heat of the anesthetic during vaporization
- (B) Delivery of diluent gas at a constant temperature regardless of flow rate
- (C) Increase of bypass flow when the vaporizer is cooled by high fresh gas flow
- (D) Maintenance of constant anesthetic vapor output over a range of vaporizer temperatures
- (E) Maintenance of constant vapor concentrations at low flow rates
Leakage current and microshock hazards are eliminated by
- (A) an isolation transformer
- (B) conductive flooring
- (C) a three-wire grounding system
- (D) a line-isolation monitor
- (E) none of the above
Which of the following combinations of anesthetic and incorrect vaporizer results in the smallest error in delivered concentration?
- (A) Sevoflurane in a halothane vaporizer
- (B) Sevoflurane in an isoflurane vaporizer
- (C) Halothane in a desflurane vaporizer
- (D) Isoflurane in a halothane vaporizer
- (E) Sevoflurane in a desflurane vaporizer
An anesthesia machine is set to deliver oxygen 2 L/min, nitrous oxide 2 L/min, and sevoflurane. After 30 minutes of stable anesthesia, which of the following, is the most likely cause of a decrease in the oxygen analyzer reading from 50% to 30%?
- (A) A leak in the ventilator bellows
- (B) Accumulation of water on the oxygen sensor membrane
- (C) Calibration at 100% oxygen using less than 100% oxygen
- (D) Disconnection of the wall oxygen hose
- (E) Presence of the oxygen analyzer in the expiratory limb
Desflurane at a stable alveolar concentration of 7%
- (A) causes bradycardia
- (B) decreases cerebrovascular resistance
- (C) degrades in soda lime
- (D) increases systemic vascular resistance
- (E) stimulates the respiratory centers
During extracorporeal shock wave lithotripsy, the shock wave should be synchronized with
- (A) the P wave of the ECG
- (B) the R wave of the ECG
- (C) the T wave of the ECG
- (D) peak inspiration
- (E) end-expiration
The accuracy of oxyhemoglobin saturation determined by digital pulse oximetry is affected significantly by each of the following EXCEPT
- (A) movement of the patient
- (B) isovolemic hemodilution to a hematocrit of 23%
- (C) position of the operating room light
- (D) intravenous administration of methylene blue
- (E) infusion of phenylephrine
During laser microsurgery of the larynx using an endotracheal tube, a fire occurs in the airway. Which of the following is the most appropriate initial management?
- (A) Increase FiO2 to 1.0
- (B) Instill saline into the endotracheal tube
- (C) Perform cricothyroidotomy
- (D) Remove the endotracheal tube
- (E) Ventilate with air
A 5-year-old boy is to undergo microlaryngeal carbon dioxide laser vaporization of laryngotracheal papillomas under halothane administered through a small polyvinylchloride (PVC) endotracheal tube. The diluent gas mixture LEAST likely to support laser combustion of the PVC tube is
- (A) oxygen 40%, nitrous oxide 60%
- (B) oxygen 25%, nitrous oxide 75%
- (C) oxygen 30%, nitrogen 70%
- (D) oxygen 30%, helium 70%
- (E) oxygen 30%, air 70%
An air/oxygen blender with E-size cylinders is supplying gas to a Mapleson D circuit being used to ventilate a neonate during transport. The air tank is full (psi= 1900/625 L) and flow is 4 L/min. The oxygen tank flow is 5 L/min and the pressure gauge indicates 500 psi. If the flow rates remain unchanged, which of the following statements is correct?
- (A) The air tank will be empty in 90 minutes
- (B) The oxygen tank will be empty in 30 minutes
- (C) The concentration of oxygen in the circuit is 60%
- (D) The oxygen tank will fill with air when the pressure gauge falls below 50 psi
- (E) The volume of oxygen remaining can be determined only by weighing the tank
An otherwise healthy 20-year-old man undergoes laser surgery for vocal cord polyp removal. During jet ventilation with 100% oxygen, arterial blood gas analysis shows PaO2 90 mmHg, PaCO2 40 mmHg, and pH 7.40. Which of the following is the most likely explanation?
- (A) Aspiration of gastric contents
- (B) Atelectasis
- (C) Pneumothorax
- (D) Pulmonary embolism
- (E) Room air entrainment
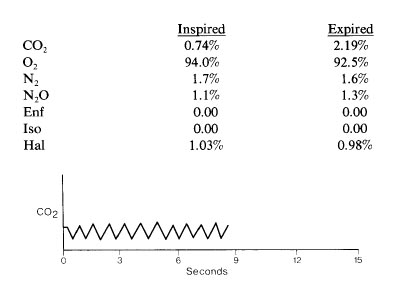
A normal adult is receiving general anesthesia via a standard circle system and controlled ventilation. Mass spectrometer data are shown. Which event is most compatible with these data?
- (A) Endobronchial intubation
- (B) Hemorrhagic shock
- (C) Incompetent expiratory valve
- (D) Substantial decrease in fresh gas flow
- (E) Venous air embolism
Which of the following decreases dead space in an anesthetic circle system?
- (A) Larger surface area of the expiratory unidirectional valve
- (B) Placing a septum in the Y-piece
- (C) Shorter expiratory limb tubing
- (D) Smaller carbon dioxide absorber
- (E) Smaller reservoir bag
Each of the following factors may lead to erroneous readings using pulse oximetry EXCEPT
- (A) electrocautery
- (B) high cardiac output states
- (C) infrared lights near the sensor
- (D) intravenous dyes
- (E) severe hemodilution
During induction of general anesthesia in a patient with a supraglottic tumor, both intubation and subsequent ventilation via a face mask are impossible. A cricothyroidotomy is performed with a 16-gauge intravenous catheter. Which of the following statements is true?
- (A) Application of pressures greater than 35 cmH2O to the catheter will increase the risk for pulmonary barotrauma
- (B) PaC02 can be maintained at a normal level using a standard circle system attached to the catheter
- (C) PaO2 greater than 100 mmHg can be maintained indefinitely using transtracheal jet ventilation with pure oxygen through the catheter
- (D) Emergency surgical tracheostomy would have improved the likelihood of survival
- (E) The presence of this tumor contraindicates jet ventilation via cricothyroidotomy
An otherwise healthy 16-year-old girl is undergoing posterior spinal fusion for thoracolumbar scoliosis. During the procedure, the most likely cause of a marked decrease in the amplitude of the somatosensory evoked potentials after stimulation of the posterior tibial nerve is
- (A) administration of fentanyl 30 jag /kg for induction
- (B) administration of isoflurane 1.3 MAC for maintenance
- (C) administration of vecuronium 0.15 mg/kg
- (D) a decrease in body temperature from 37 to 35°C
- (E) a decrease in cerebrospinal fluid pressure
The pin index system
- (A) is not used in central pipeline connections
- (B) requires aligning four pins with four holes
- (C) is used on all sizes of medical gas cylinders
- (D) has been replaced by color coding of gas cylinders
- (E) prevents overfilling of gas cylinders
Following antagonism of a nondepolarizing muscle relaxant with neostigmine, twitch height is normal. To achieve this effect, the percentage of the acetylcholine receptor pool that must be free of muscle relaxant is
- (A) 10
- (B) 25
- (C) 33
- (D) 50
- (E) 75
A 30-kg patient with asthma is receiving general anesthesia and being mechanically ventilated with a measured tidal volume of 300 mL. Increasing the fresh gas flow from 3 L/min to 9 L/min without changing the ventilatory rate or I:E ratio will result in
- (A) decreased physiologic dead space
- (B) increased delivered tidal volume
- (C) increased end-expired carbon dioxide
- (D) unchanged delivered minute volume
- (E) unchanged peak inspiratory pressure
During steady-state intraoperative controlled mechanical ventilation, exhaled tidal volume will be increased by
- (A) changing to more compliant tubing in the ventilatory circuit
- (B) increasing fresh gas flow in the anesthesia machine
- (C) increasing nitrous oxide concentration in the inspired mixture
- (D) increasing ventilatory rate
- (E) moving the volume sensor as far as possible from the patient
Which of the following detects the smallest volume of venous air embolization?
- (A) Changing the precordial Doppler ultrasound signal
- (B) Decreasing PetC02
- (C) Decreasing Sp02
- (D) Increasing central venous pressure
- (E) Increasing pulmonary artery pressure
A healthy 57-year-old man with a ureteral calculus is scheduled for immersion extracorporeal shock wave lithotripsy. Which of the following statements is true?
- (A) Delivery of the shock wave is timed by the R wave of the ECG
- (B) Continuous epidural anesthesia is contraindicated because of the risk for infection
- (C) If a regional technique is used, a T10 sensory level is required for adequate anesthesia
- (D) If general anesthesia is used, high tidal volumes and low respiratory rate are preferred
- (E) Removal of the patient from the bath is accompanied by an increase in blood pressure
Which Mapleson breathing circuit permits the LEAST amount of fresh gas inflow to prevent rebreathing during spontaneous ventilation?
- (A) A
- (B) B
- (C) C
- (D) D
- (E) E
Which of the following vaporizer filling errors is most likely to result in inadvertent anesthetic overdose?
- (A) Sevoflurane in a halothane vaporizer
- (B) Sevoflurane in an isoflurane vaporizer
- (C) Halothane in an sevoflurane vaporizer
- (D) Halothane in an isoflurane vaporizer
- (E) Isoflurane in an sevoflurane vaporizer
Which of the following statements concerning monitoring of neuromuscular function during general anesthesia is true?
- (A) Facial nerve electrodes underestimate recovery from block, compared with ulnar nerve electrodes
- (B) More current is required to depolarize a nerve beneath the negative electrode than beneath the positive electrode
- (C) Needle electrodes should be electrically grounded
- (D) Supramaximal voltage is 10% higher than the voltage required to elicit pain in the awake patient
- (E) The amount of neuromuscular block is underestimated if electrodes are placed on a paretic limb
The vapor pressure of a volatile anesthetic depends on
- (A) temperature only
- (B) ambient pressure only
- (C) temperature and ambient pressure
- (D) pressure and volume of the system
- (E) none of the above
Proper zeroing of an arterial pressure transducer attached to a supine anesthetized patient is best accomplished by
- (A) continuous flow of fluid through the intravascular catheter
- (B) opening the system to air at heart level
- (C) placement of the transducer diaphragm at heart level
- (D) proper damping of the transducer system
- (E) zeroing the transducer during the expiration phase of mechanical ventilation
An arterial blood sample is obtained from a patient undergoing hypothermic cardiopulmonary bypass at 28 C. Analysis at 37 C shows a pH of 7.40 and PaCO2 of 40 mmHg. Which of the following values are most likely if the analysis is corrected to 28 C?
- (A) pH = 7.40; PaCO2 = 40
- (B) pH > 7.40; PaCO2 < 40
- (C) pH > 7.40; PaCO2 > 40
- (D) pH < 7.40; PaCO2 < 40
- (E) pH < 7.40; PaCO2 > 40
When inspired anesthetic gases are humidified
- (A) most particles 1 to 2 microns in size are deposited in the trachea
- (B) respiratory epithelial cilia become less active
- (C) alveolar water vapor pressure is unchanged
- (D) respiratory heat loss is abolished
- (E) sterilization of breathing apparatus is mandatory
Desflurane is delivered using a vaporizer that contains internal heaters because
- (A) heat decreases the drug's viscosity
- (B) heat reduces thermal loss in the patient
- (C) heat increases the drug's oil-gas partition coefficient
- (D) heat prevents fluctuations of vapor pressure
- (E) it does not vaporize adequately at room temperature
Which of the following statements concerning the check valve of the common gas outlet on an anesthesia gas machine is true?
- (A) It prevents backflow into vaporizers
- (B) It prevents delivery of a hypoxic mixture
- (C) It prevents rebreathing
- (D) It is located downstream from the oxygen flush valve
- (E) It is required for proper functioning of the proportioning system
A healthy patient is receiving general endotracheal anesthesia with nitrous oxide 4 L/min, oxygen 2 L/min, and isoflurane 1% with spontaneous ventilation. The inspiratory breathing hose becomes disconnected from the inspiratory valve. The earliest alarm will be produced by
- (A) a pulse oximeter with finger probe set to alarm at 60% saturation
- (B) a mass spectrometer set to alarm when no breath is detected for 30 seconds
- (C) an oxygen analyzer mounted on the inspiratory valve outlet and set to alarm at 25% oxygen concentration
- (D) a capnograph sensor at the Y-piece that alarms when end-tidal carbon dioxide tension is greater than 60
- mmHg
The tracing shown is from a femoral artery catheter. Which of the following is the most likely explanation?
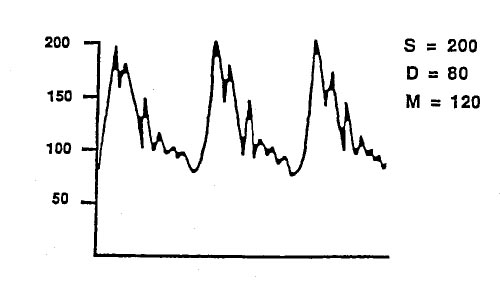
- (A) An air bubble greater than 1 ml is in the tubing
- (B) The diastolic pressures is factitiously high
- (C) Mean blood pressure is inaccurate
- (D) The monitoring system is underdamped
- (E) Systolic pressure in the aortic arch exceeds 200 mmHg
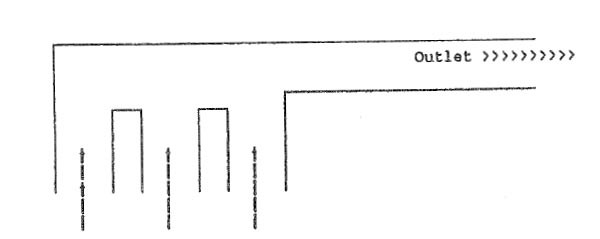
In this diagram of a circle system, an increase in dead space is most likely to result from placement of the pressure relief valve at location
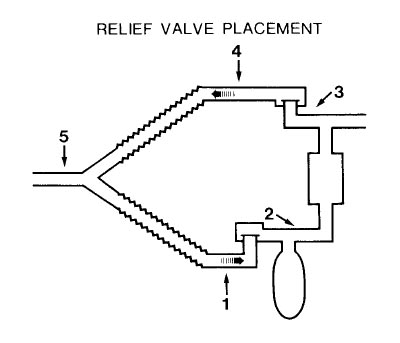
- (A) 1
- (B) 2
- (C) 3
- (D) 4
- (E) 5
During anesthesia with nitrous oxide, oxygen, and a relaxant, the patient's lungs are being mechanically ventilated and there is a heated humidifier in the circuit. The most likely cause of an apparent increase in inspired oxygen concentration is
- (A) a hole in the ventilator bellows
- (B) backflow of fresh gas because of resistance in the humidifier
- (C) decreased oxygen utilization by the patient
- (D) heat damage to the oxygen sensor
- (E) water condensation on the oxygen sensor
Which of the following is the greatest disadvantage of pressure-cycled ventilation?
- (A) Increased I:E ratio
- (B) Increased mechanical dead space
- (C) Increased risk for barotrauma
- (D) Variable respiratory rates
- (E) Variable tidal volumes
Pulmonary artery occlusion pressure
- (A) does not reliably reflect left ventricular end-diastolic volume when left ventricular compliance is reduced
- (B) inaccurately reflects left atrial pressure when left atrial pressure exceeds 15 mmHg
- (C) is measured at end-inspiration in mechanically ventilated patients
- (D) overestimates left atrial pressure in patients with poor lung compliance
- (E) reflects left atrial pressure only if the catheter tip is located in zone II of the lung
A 55-year-old man is undergoing craniotomy in the sitting position. Mean arterial pressure is 75 mmHg; arterial blood gas values are PaCO2 41 mmHg and pH 7.37. End-tidal CO2 is 7 mmHg. Which of the following is the most likely cause of the increased PaCO2 to PetCO2 gradient?
- (A) Decreased cardiac output
- (B) Endobronchial intubation
- (C) Hyperinflation of the lungs
- (D) Partial disconnect of the capnograph sample tubing
- (E) Venous air embolism
In the event of a leak in the air flowmeter, which flowmeter arrangement produces the lowest risk of delivering hypoxic gas mixtures?
- (A) Air, O2, N2O
- (B) N2O, O2, Air
- (C) N2O, Air, O2
- (D) O2, Air, N2O
- (E) O2, N2O, Air
Measurement of blood pressure with a Doppler device involves
- (A) reflection of ultrasound waves off blood elements
- (B) detection of oscillations in cuff pressure
- (C) amplification of Korotkoff sounds with a miniature microphone
- (D) transillumination with a near infrared light
- (E) detection of variations in blood vessel diameter
The gauge pressure on a cylinder of nitrous oxide
- (A) varies with the size of the cylinder
- (B) is the same for full and half-full cylinders
- (C) is the same as that of a full cylinder of oxygen if both are full
- (D) is independent of the temperature of the cylinder
- (E) reliably indicates the amount of nitrous oxide in the cylinder
Which of the following statements concerning absorption of carbon dioxide by soda lime in an anesthetic circuit is correct?
- (A) A warm canister indicates reserve absorption capability
- (B) Fresh soda lime includes calcium carbonate
- (C) Intergranular volume of the canister should exceed the patient's tidal volume
- (D) The color indicator is methylene blue
- (E) The reaction removes water
In the operating room
- (A) conductive floors are necessary for electrical safety
- (B) the ECG monitor may be used as a grounding source
- (C) an improperly grounded electrocautery causes ventricular fibrillation
- (D) an isolation transformer offers no protection against microelectrocution
- (E) a line isolation monitor will interrupt power automatically if excessive leakage to ground is detected
A Fluotec vaporizer is set to administer halothane 4% using a fresh gas flow of 4 L/min. If the diluent gas flow is increased to 8 L/min, and at the same time the room temperature increases from 20 to 25°C, the approximate concentration of halothane delivered to the patient would be
- (A) 2%
- (B) 2.5%
- (C) 3%
- (D) 4%
- (E) 5%
Which of the following is most effective in decontaminating an anesthesia machine that was splattered with HIV-contaminated blood?
- (A) Bleach
- (B) Deionized water
- (C) Ethylene oxide
- (D) Hydrogen peroxide
- (E) Isopropyl alcohol
Recommendations for maximal allowable trace anesthesia gases are based on
- (A) achievable levels with modern scavenging systems
- (B) data from animal studies
- (C) data on methionine synthetase levels in anesthesiologists
- (D) evidence for an association with malignancy in anesthesiologists
- (E) evidence for an association with spontaneous abortion In operating room personnel
During induction of anesthesia, a patient is breathing isoflurane from a semiclosed circle absorber system. The temperature-compensated vaporizer is set to deliver isoflurane 1.5%. Which of the following will result in the lowest inspired concentration of isoflurane?
- (A) Doubling the length of circle system hoses
- (B) Decreasing the barometric pressure
- (C) Changing from rubber to plastic breathing hoses
- (D) Decreasing fresh gas flow
- (E) Exhaustion of the soda lime
A 75-year-old man with a left bundle branch block is undergoing placement of a pulmonary artery catheter through the right internal jugular vein. He becomes pale and his heart rate decreases to 40 bpm when the catheter tip enters the right ventricle. The most likely cause is
- (A) a catheter loop in the right atrium
- (B) acute myocardial infarction
- (C) acute pneumothorax
- (D) carotid sinus reflex
- (E) complete heart block
A pulmonary artery catheter is placed in an awake patient breathing room air. Typical right ventricular and pulmonary artery pressure tracings are obtained. With the catheter balloon inflated, blood drawn from the distal port has a PaO2 of 100 mmHg, while a simultaneous radial artery sample has a PaO2 of 90 mmHg. These data indicate that the
- (A) shunt fraction is greater than 10%
- (B) catheter is in the wedged position
- (C) catheter has entered a pulmonary vein
- (D) cardiac output is abnormally high
- (E) oxygen electrode is malfunctioning
On routine inspection of an anesthesia machine, the nitrous oxide E cylinder pressure is 360 psi. This indicates that the
- (A) pressure in the cylinder is 16 atm
- (B) cylinder contains no liquid nitrous oxide
- (C) cylinder is half full
- (D) cylinder contains enough nitrous oxide for one hour of anesthesia at a flow rate of 3 L/min
- (E) reducing valve is malfunctioning
One full E-cylinder of oxygen at 20°C can deliver 2 L/min of oxygen for at most
- (A) 30 minutes
- (B) 90 minutes
- (C) 3 hours
- (D) 5 hours
- (E) 12 hours
Which of the following will occur if the top of the oxygen flowmeter is cracked and leaking during anesthesia with nitrous oxide and oxygen?
- (A) The back-pressure check valve will protect against a hypoxic gas mixture
- (B) The fail-safe mechanism will protect against a hypoxic gas mixture
- (C) The inspired oxygen concentration will be less than that set by the flowmeters
- (D) The leak will be detected if the circle is pressurized prior to use
- (E) The rotameter will accurately reflect the fresh gas flow to the patient
After inflation of both the tracheal and endobronchial cuffs of a left-sided double-lumen tube, the following are noted on auscultation of the chest: Left lumen clamped --> Breath sounds absent bilaterally; Right lumen clamped --> Breath sounds present on left only; Both lumens open --> Breath sounds present on left only. The most appropriate action is to
- (A) decrease the endobronchial cuff volume
- (B) decrease the tracheal cuff volume
- (C) reinsert the tube, rotating it 180 degrees to the right
- (D) suction both lumens
- (E) withdraw the tube slightly and repeat the auscultory maneuvers
An sevoflurane vaporizer is filled with isoflurane and the vaporizer dial is set at 1%. Which of the following will occur?
- (A) Less than 1% isoflurane will be delivered
- (B) More than 1% isoflurane will be delivered
- (C) Thymol precipitation will prevent vaporization
- (D) The vaporizer bypass will not open
- (E) The vaporizer will be damaged
Reduction of fire hazards during laser surgery of the airway is best accomplished by use of
- (A) continuous mode laser emissions
- (B) a nitrous oxide/opioid/relaxant anesthetic technique
- (C) a polyvinylchloride endotracheal tube and cuff
- (D) topical lidocaine
- (E) saline-filled sponges over exposed tissues
A patient whose trachea is intubated develops partial airway obstruction two hours after induction of fentanyl, nitrous oxide, oxygen anesthesia. The anesthesiologist discontinues the nitrous oxide and controls ventilation, and there is gradual improvement during the next hour. No evidence of a respiratory disorder is found at the conclusion of the anesthetic. Which of the following is most likely?
- (A) The endotracheal tube was in the right mainstem bronchus
- (B) The patient had an unrecognized air embolism
- (C) The patient had a nitrous oxide pneumothorax
- (D) The endotracheal tube cuff narrowed the airway
- (E) The fentanyl induced chest rigidity
Postoperatively, a patient is being mechanically ventilated by a constant-flow, pressure-cycled ventilator with the following initial settings: inspiratory/expiratory (I/E) ratio of 1:2, peak inspiratory pressure (PIP) of 25 cmH2O, and rate of 10/min. One hour later, the I/E ratio is 1:4. Which of the following would ensure that the minute ventilation is the same as that initially set?
- (A) Inflate the endotracheal tube cuff to prevent leakage
- (B) Double the respiratory rate
- (C) Decrease the expiratory pause until the I/E ratio is 1.0
- (D) Increase the PIP until the I/E ratio is 1:2
- (E) Increase the PIP to 50 cmH20
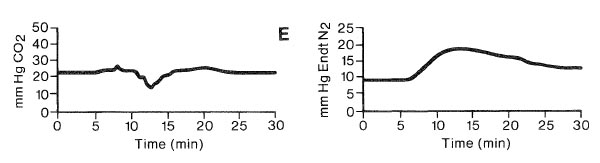
A 2-year-old child has cardiac arrest during an inguinal herniorrhaphy under general anesthesia administered during a Jackson-Rees system. The graph shows end-tidal PCO2 monitored from the tip of the endotracheal tube during cardiopulmonary resuscitation; minute ventilation is unchanged. Which of the following is the most likely cause of the change beginning at the arrow?
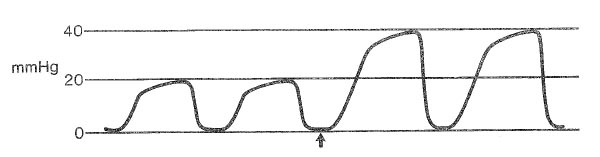
- (A) Decreased fresh gas flow
- (B) Inadequate chest compression
- (C) Increased dead space
- (D) Restoration of cardiac output
- (E) Sampling artifact
With direct arterial blood pressure monitoring
- (A) systolic pressure in the aortic root exceeds that in the radial artery
- (B) mean and diastolic pressures are lower in the dorsalis pedis artery than in the aortic root
- (C) the dicrotic notch is not clearly found on femoral arterial waveforms
- (D) an underdamped waveform is characteristic of bubbles in the system
- (E) longer tubing between artery and transducer artifactually augments systolic pressure
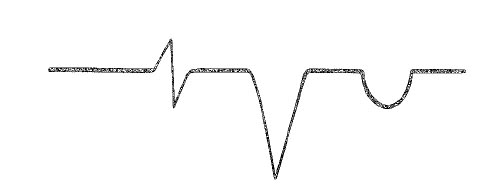
The most likely cause of this capnographic tracing obtained just after laryngoscopy and intubation is
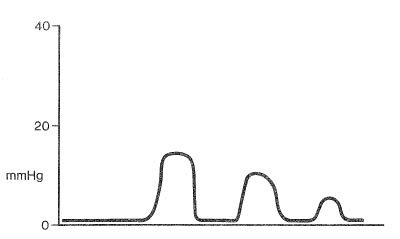
- (A) esophageal intubation
- (B) partial obstruction of the endotracheal tube
- (C) pulmonary embolus
- (D) insertion of an endotracheal nasogastric tube
- (E) mild bronchospasm
During anesthesia using the Bain circuit
- (A) PaCO2 is independent of minute volume if fresh gas flow is greater than 17 ml/kg
- (B) PaCO2 is independent of fresh gas flow if minute volume is greater than 100 ml/kg
- (C) PaCO2 may be normal in the presence of rebreathing
- (D) carbon dioxide removal is more efficient during spontaneous ventilation than during controlled ventilation
- (E) less body heat is lost than with a circle system
Which of the following statements concerning use of a Bain circuit is true?
- (A) Fresh gas flow can be as low as the patient's minute ventilation
- (B) Heat conservation is better than with a circle system
- (C) Lower flows can be used with controlled ventilation than with spontaneous ventilation
- (D) Lower fresh gas flows can be used than with a Jackson-Rees system
- (E) The concentration of inspired vapors can be changed rapidly
Oxygen 100 ml/min is bubbled through a vaporizer containing an anesthetic with a vapor pressure of 150 mmHg, and this mixture is added to a fresh gas flow of 5 L/min. The delivered anesthetic concentration is
- (A) 0.25%
- (B) 0.5%
- (C) 1%
- (D) 2.5%
- (E) 5%
The jet ventilation technique using an injector during laryngobronchoscopy relies on
- (A) air entrainment
- (B) relative density of inhaled gases
- (C) presence of an endotracheal tube
- (D) presence of spontaneous ventilation
- (E) use of helium-oxygen mixtures
The principal rationale for the use of warmed humidified inspired anesthetic gases in children is to
- (A) decrease postoperative respiratory complications
- (B) decrease postoperative shivering
- (C) preserve ciliary function
- (D) prevent dehydration
- (E) prevent evaporative heat loss
Which Mapleson breathing circuit shown in the illustration permits the LEAST amount of fresh gas inflow to prevent rebreathing during spontaneous ventilation?
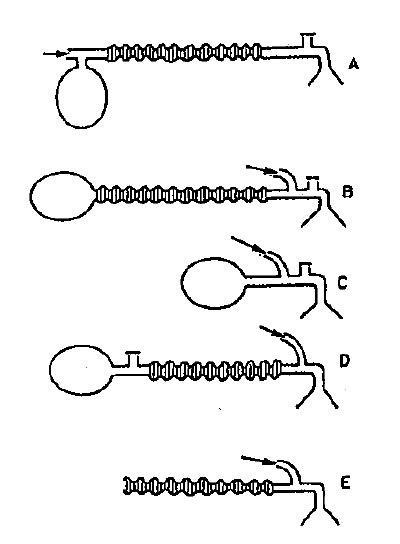
- (A) A
- (B) B
- (C) C
- (D) D
- (E) E
Which of the following is characteristic of soda lime and Baralyme carbon dioxide absorption canisters used in circle systems?
- (A) Calcium carbonate is a major end product
- (B) Carbon dioxide absorption cools the anesthetic gases
- (C) Flushing the canister with oxygen for six hours will regenerate 50% of the spent Baralyme
- (D) Gases lose water vapor as they pass through the canisters
- (E) Soda lime and Baralyme depend on silica as a binding agent
During direct intra-arterial measurement of blood pressure
- (A) the mean arterial pressure will be unaffected by small air bubbles in the system
- (B) an underdamped system will overestimate the mean arterial pressure
- (C) an underdamped system will overestimate the diastolic pressure
- (D) long tubing from the catheter to the transducer will tend to decrease resonance in the system
- (E) calibration of the transducer by opening a stopcock to air at the sternal angle will overestimate the mean
During attempted cannulation of the right internal jugular vein, the exploring needle goes lateral to the vein. Which of the following structures is most likely to be encountered?
- (A) Carotid artery
- (B) Vagus nerve
- (C) Thoracic duct
- (D) Phrenic nerve
- (E) Long thoracic nerve
Which of the following is most effective in preventing intraoperative hypothermia in adults?
- (A) Heating and humidifying inspired gases
- (B) Maintaining a warm operating room
- (C) Using a circulating warm-water mattress
- (D) Using reflective coverings
- (E) Warming intravenous fluids
A burn is found at the site of the electrocautery pad. Which of the following is most likely?
- (A) The electrosurgical unit was in the bipolar mode
- (B) The electrocautery pad became partially detached
- (C) The electrosurgical unit ground wire was severed
- (D) The line-isolation monitor alarmed
- (E) The patient became grounded
The two E oxygen cylinders on an anesthesia machine have pressure readings of 1100 psi each. At an oxygen flow of 3 L/min, there will be sufficient oxygen for approximately
- (A) 2.5 hours
- (B) 3.5 hours
- (C) 5.5 hours
- (D) 7 hours
- (E) 8 hours
A radial artery catheter is to be used for blood pressure measurement during a sitting craniotomy. When zeroing the transducer, which of the following describes the best levels for placement of the transducer and opening of the system to air? (Transducer, Opening to Air)
- (A) Head Wrist
- (B) Head Head
- (C) Head Heart
- (D) Heart Heart
- (E) Heart Wrist
To detect the delivery of a hypoxic gas mixture, the optimal location for an oxygen analyzer in this circle is
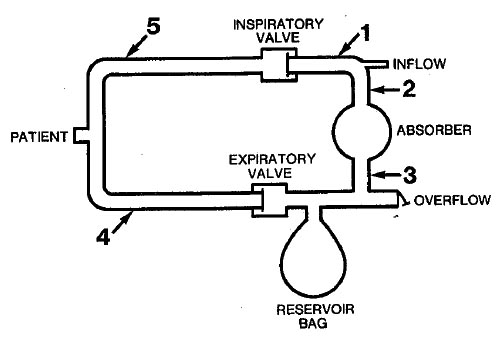
- (A) 1
- (B) 2
- (C) 3
- (D) 4
- (E) 5
A 35-kg child requires mechanical ventilation with pure oxygen at a tidal volume of 350 ml and a rate of 20/min during a severe asthma attack. The most likely cause of severe hypotension after initiating mechanical ventilation is
- (A) hypoxic circulatory depression
- (B) inadequate expiratory time
- (C) increased pulmonary vascular resistance
- (D) respiratory alkalosis
- (E) tension pneumothorax
Which property of oxygen is detected by the fail-safe device on the anesthesia machine?
- (A) Concentration
- (B) Flow
- (C) Pressure
- (D) Partial pressure
- (E) Reserve volume
While checking an anesthesia machine, opening the oxygen flow-control valve yields no oxygen flow, although the wall-mounted oxygen pipeline supply gauge reads 50 psig. Opening the backup oxygen cylinder results in normal oxygen flow. The most likely cause is
- (A) failure of the oxygen pipeline supply
- (B) failure of the second-stage oxygen pressure regulator
- (C) a malfunctioning check valve in the oxygen pipeline supply inlet
- (D) a malfunctioning fail-safe valve
- (E) a malfunctioning oxygen flow-control valve
The trend plot shows end-tidal gases measured during a radical neck dissection. The event occurring at A is most likely
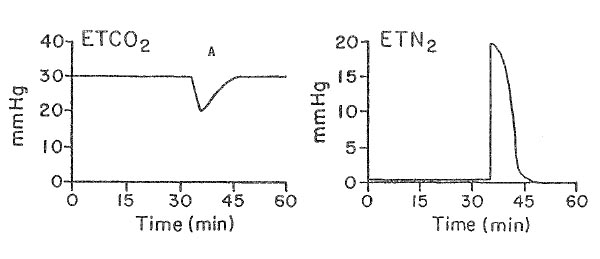
- (A) acute hypotension
- (B) endobronchial intubation
- (C) kinking of the endotracheal tube
- (D) rupture of the endotracheal cuff
- (E) venous air embolism
After removing the electrocautery pad from the thigh, a burn is noted at that site. Which of the following most likely contributed to this injury?
- (A) A line-isolation monitor fault
- (B) Current leak from the EKG module
- (C) Defective grounding of the electrocautery unit
- (D) Dried gel on the electrocautery pad
- (E) Excessive current setting for cutting mode
During laser excision of a vocal cord polyp, the tracheal tube ignites. Which of the following is the most appropriate next step?
- (A) Continue ventilation with air
- (B) Ensure patency of the endotracheal tube
- (C) Extubate the trachea
- (D) Flood the surgical field with saline solution
- (E) Increase the concentration of nitrous oxide
An unconscious adult patient is being ventilated through an esophageal obturator airway (EOA) in the emergency department. In the absence of cervical spine injury, which of the following is appropriate?
- (A) Use of the EOA for airway management until the patient regains consciousness
- (B) Removal of the EOA before insertion of an endotracheal tube
- (C) Placement of an endotracheal tube before removal of the EOA
- (D) Removal of the EOA under fiberoptic endoscopic visualization
- (E) Cricothyroidotomy
Intraoperatively, the occurrence of prominent "a" waves on the central venous pressure waveform can be explained by each of the following EXCEPT
- (A) acute right ventricular failure
- (B) atrial flutter
- (C) complete heart block
- (D) onset of junctional tachycardia
- (E) ventricular pacing
While delivering nitrous oxide 1.5 L/min, oxygen 1.5 L/min, and sevoflurane 2%, a leak in the oxygen flowmeter would most likely be detected by the
- (A) low airway pressure alarm
- (B) "fail-safe" system
- (C) oxygen analyzer on the expiratory limb
- (D) oxygen flowmeter reading
- (E) mass spectrometric analysis of gases
Which of the following neurophysiologic monitoring modalities is LEAST affected by administration of volatile anesthetic agents?
- (A) Brain stem auditory evoked potentials
- (B) Electroencephalogram
- (C) Motor evoked potentials
- (D) Somatosensory evoked potentials
- (E) Visual evoked potentials
During laser excision of vocal cord polyps in a 5-year-old boy, dark smoke suddenly appears in the surgical field. The trachea is intubated and anesthesia is being maintained with halothane, nitrous oxide, and oxygen. The most appropriate initial step is to
- (A) change from oxygen and nitrous oxide to air
- (B) fill the oropharynx with water
- (C) instill water into the endotracheal tube
- (D) remove the endotracheal tube
- (E) ventilate with carbon dioxide
The flow proportioning system on an anesthesia machine
- (A) is regulated primarily by changes in oxygen input pressure
- (B) limits nitrous oxide flow when oxygen pressure falls below a preset value
- (C) maintains a minimum ratio of oxygen to nitrous oxide in fresh gas flow
- (D) precludes the use of a closed system
- (E) regulates flows of oxygen and nitrous oxide to maintain a fixed FlO:
During surgery with a carbon dioxide laser, which inhaled gas mixture is LEAST likely to promote combustion of the endotracheal tube?
- (A) Oxygen 25%-helium 75%
- (B) Oxygen 25%-nitrogen 75%
- (C) Oxygen 25%-nitrous oxide 75%
- (D) Oxygen 50%-nitrogen 50%
- (E) Oxygen 50%-nitrous oxide 50%
Two opened oxygen cylinders, one full and one empty, are attached to an anesthesia machine. The check valve to the empty cylinder fails. This is expected to result in
- (A) activation of the fail-safe device
- (B) cessation of oxygen flow to the anesthesia circuit
- (C) filling of the empty cylinder with a mixture of all gases supplied to the anesthesia machine
- (D) increase in the temperature of the empty cylinder
- (E) interruption of gas delivery from the central oxygen source
A waste-gas scavenger has an active disposal system. Which of the following safety features is necessary to prevent removal of excess gas from the breathing circuit?
- (A) Positive-pressure relief mechanism
- (B) Negative-pressure relief mechanism
- (C) Low-volume scavenging reservoir
- (D) High-volume scavenging reservoir
- (E) Maximum vacuum flow rate of 5 L/min
An 88-kg man is anesthetized with 66% nitrous oxide, 33% oxygen, and 1% isoflurane using a circle system. Following tracheal intubation, the nitrous oxide flow is set at 1 L/min and the oxygen flow is set at 0.5 L/min. After two hours the oxygen monitor indicates a circuit oxygen concentration of only 25% despite the flows noted above. The most likely explanation for this discrepancy is
- (A) decrease of oxygen pipeline pressure to 20 psi
- (B) increase in the concentration of nitrous oxide in the circuit
- (C) inaccuracy of flowmeters at low flow rates
- (D) malfunction of the oxygen monitor
- (E) progressive hypothermia
Arterial pressure in the radial artery is 155/70 mmHg measured by a correctly calibrated catheter-transducer system. At the same time aortic pressure is 140/75 mmHg using a high-fidelity catheter tip transducer. The most likely cause of this discrepancy is
- (A) a large amount of air in the dome of the radial artery transducer
- (B) coarctation of the aorta
- (C) peripheral vascular constriction produced by sympathetic stimulation
- (D) physiologic amplification of the wave form from the aorta to the radial artery
- (E) too high a frequency response in the catheter-transducer system
Proper handling of oxygen cylinders includes
- (A) maintenance of storage room temperature above 60°F
- (B) separate storage rooms for nitrous oxide and oxygen
- (C) opening the cylinder valve just sufficiently to register tank pressure accurately
- (D) storage in a room with conductive flooring
- (E) opening the cylinder valve briefly before attachment to the anesthesia machine
A 68-year-old patient is undergoing total hip replacement during general anesthesia using positive pressure ventilation and neuromuscular blockade. Intraoperative monitoring shows a gradual decrease in end-tidal CO2, an increase in exhaled tidal volume, and an increase in measured FiO2. Which of the following is the most likely cause of these changes?
- (A) Air entrainment around a deflated endotracheal tube cuff
- (B) Channeling of the exhaled air through the carbon dioxide canister
- (C) Fat embolism
- (D) Inadequate muscle relaxation with spontaneous patient ventilation
- (E) A small hole in the ventilator bellows
Maximum current is delivered to the myocardium by a countershock for defibrillation when
- (A) paddle contact pressure is minimal
- (B) petroleum jelly is used under the paddles
- (C) previous countershocks of the same power have been attempted
- (D) the patient is grounded securely
- (E) the shock is applied at the end of inspiration
The capnographic tracing is from a 2-month-old infant anesthetized using a pediatric circle system and mask at a fresh gas flow of 4 L/min. The sampling port is in the elbow connector. This tracing indicates
- (A) adequate alveolar ventilation
- (B) exhausted soda lime
- (C) expired halothane concentrations representative of alveolar concentrations
- (D) mixing of inspired and expired gases
- (E) the need to change to a Mapleson D circuit
Pulmonary artery diastolic pressure is an unreliable indicator of left ventricular end-diastolic pressure in patients with
- (A) acute cardiogenic pulmonary edema
- (B) aortic stenosis
- (C) acute mitral regurgitation
- (D) myocardial ischemia
- (E) severe emphysema
A 16-year-old child has an arterial catheter inserted prior to a potentially difficult intubation for a craniofacial operation. While awake and breathing room air, arterial blood gas values are: PaO2 134 mm Hg, PaCO2 28 mm Hg, and pH 7.45. These values can be explained by
- (A) excess heparin mixed with the arterial sample
- (B) a patient core temperature of 38°C
- (C) excess air entrained in the syringe during sampling
- (D) storing the sample at room temperature for 15 minutes before processing
- (E) anxiety and hyperventilation
A 46-year-old patient who abuses intravenous drugs develops acute aortic valvular insufficiency from bacterial endocarditis. Which of the following statements concerning pressures measured through a pulmonary artery catheter is true?
- (A) Pulmonary artery occlusion pressure will underestimate left ventricular end-diastolic pressure
- (B) Pulmonary artery oxygen saturation will overestimate mixed venous oxygen saturation
- (C) Thermodilution cardiac output determination will overestimate cardiac output
- (D) Right ventricular end-diastolic pressure will equal left ventricular end-diastolic pressure
- (E) The pulmonary artery occlusion pressure trace will most likely have large V waves
During use of the ventilator on an anesthesia machine, positive pressure is noted on the airway pressure gauge during exhalation. Positive end-expiratory pressure has not been purposefully added to the breathing circuit. Which of the following is the most likely cause?
- (A) Closure of the pop-off valve in the circle system
- (B) Excessive tidal volume settings on the ventilator
- (C) Obstruction of the pressure relief valve on the scavenging system
- (D) Overinflation of the endotracheal tube balloon
- (E) Tension pneumothorax
In a normally functioning circle anesthesia system, if the length of the inspiratory and expiratory hose is doubled, the mechanical dead space will be
- (A) halved
- (B) unchanged
- (C) doubled
- (D) quadrupled
- (E) dependent on compression volume
Cardiac output measured by thermodilution with a pulmonary artery catheter most accurately reflects systemic blood flow in a patient with
- (A) aortic regurgitation
- (B) atrial septal defect
- (C) patent ductus arteriosus
- (D) tricuspid insufficiency
- (E) ventricular septal defect
To detect the delivery of hypoxic gas mixture, the optimal location for an oxygen analyzer in this circle is
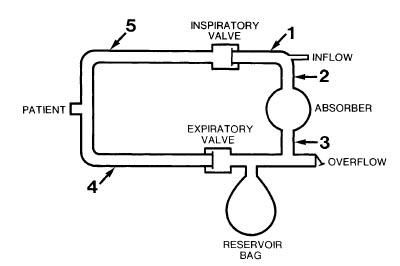
- (A) 1
- (B) 2
- (C) 3
- (D) 4
- (E) 5
Which of the following statements concerning anesthesia machine flowmeters is true?
- (A) At high gas flows, viscosity is the predominant determinant of flow rate
- (B) At low flow rates, gas density is the predominant determinant of flow rate
- (C) Flowmeters should be upstream from the oxygen fail-safe device
- (D) The oxygen flowmeter should be upstream from other flowmeters
- (E) Tapered flow tubes allow a constant decrease in pressure across the float
An isoflurane-specific vaporizer that is 25% full is mistakenly refilled with halothane, and the dial is set at 1.5%. Which of the following statements concerning this situation is true?
- (A) The gas mixture will contain equal partial pressures of halothane and isoflurane
- (B) The gas mixture will produce a greater depth of anesthesia than 1.5% isoflurane alone
- (C) The gas mixture will produce a greater depth of anesthesia than 1.5% halothane alone
- (D) The liquid mixture will have a higher vapor pressure than 1.5% halothane alone
- (E) The liquid mixture will have a higher vapor pressure if it is placed in a halothane-specific vaporizer
A 32-year-old woman is anesthetized for suboccipital craniotomy. During positioning, the capnograph shows an abrupt decrease in the slope of the expiratory upstroke. Which of the following is the most likely cause?
- (A) Air embolism
- (B) Incompetent expiratory valve
- (C) Incomplete neuromuscular block
- (D) Kinked endotracheal tube
- (E) Tracheal extubation
When using a Venturi face mask with a reservoir bag
- (A) a known constant FiO2 is delivered
- (B) the reservoir bag ensures predictable FiO2 while conserving fresh gas flow
- (C) low fresh gas flows will not decrease FiO2
- (D) the system prevents hypocarbia during tachypnea
- (E) the system increases anatomic dead space
Compared with a semiclosed circle system, a closed system
- (A) decreases the risk for anesthetic overdose
- (B) decreases the risk for rebreathing carbon dioxide
- (C) has lower resistance to gas flow
- (D) permits calculation of oxygen consumption
- (E) permits more rapid changes in anesthetic depth
A child undergoing general anesthesia is breathing spontaneously using the Jackson-Rees modification of the Ayres T-piece. Respiratory rate is 20/min and tidal volume is 75 ml. What is the minimum fresh gas flow required to prevent rebreathing?
- (A) 750 ml/min
- (B) 1500 ml/min
- (C) 2250 ml/min
- (D) 4500 ml/min
- (E) 6000 ml/min
During general anesthesia using a modern anesthesia machine, a patient's spontaneous ventilation is manually assisted with a fresh gas flow of 5 L/min. A sudden malfunction of the pressure-relief (pop-off) valve of the circle absorption system occurs, and the valve cannot be opened. The most appropriate next step is to
- (A) change to a smaller reservoir bag
- (B) increase total fresh gas flow
- (C) open the scavenger valve
- (D) control ventilation manually
- (E) switch to mechanical ventilatory mode
The two E oxygen cylinders on an anesthesia machine have pressure readings of 1100 psi each. At an oxygen flow of 3 L/min, there will be sufficient oxygen for approximately
- (A) 2.5 hours
- (B) 3.5 hours
- (C) 5.5 hours
- (D) 7 hours
- (E) 8 hours
The Bain circuit
- (A) provides nearly identical delivered and inspired anesthetic concentrations
- (B) has the fresh gas flow inlet near the reservoir bag
- (C) is a nonrebreathing circuit at any fresh gas flow rate
- (D) is most efficient during spontaneous ventilation
- (E) has a time constant greater than 1 minute for change in inspired anesthetic concentrations
During general anesthesia administered through a circle system, the soda lime absorbant is exhausted. No fresh soda lime is available for use. Which of the following is the most appropriate next step to prevent hypercapnia in this patient?
- (A) Decreasing the dead space of the circle system
- (B) Discontinuing nitrous oxide
- (C) Increasing the fresh gas flow
- (D) Increasing tidal volume
- (E) Switching to spontaneous ventilation
Which of the following is the most appropriate action after an anesthetic vaporizer is tipped?
- (A) Return to the manufacturer for recalibration
- (B) Flush the vaporizer with oxygen at 5 L/min for 24 hours
- (C) Store the vaporizer for 24 hours at room temperature
- (D) Set the vaporizer at low concentration and flush with oxygen at 10 L/min for 30 minutes
- (E) Verify the vaporizer output with mass spectrography
The lungs of a 7-kg infant are being ventilated with a volume-cycled ventilator at a rate of 20/min. The anesthetic circuit has a compressible volume of 5 ml/cm H2O, and the peak inspiratory pressure is 20 cmH2O. To achieve adequate ventilation, the ventilator tidal volume should be set at
- (A) 50 ml
- (B) 125 ml
- (C) 175 ml
- (D) 225 ml
- (E) 300 ml
While delivering nitrous oxide 1.5 L/min, oxygen 1.5 L/min, and halothane 1%, a leak in the oxygen flowmeter will most likely be detected by the
- (A) low airway pressure alarm
- (B) "fail-safe" system
- (C) oxygen analyzer on the expiratory limb
- (D) oxygen flowmeter reading
- (E) mass spectrometric analysis of gases