121 questions match your search.
When succinylcholine is administered intravenously to infants, intragastric pressure
- (A) is usually unchanged
- (B) increases to a peak of 30 cmH20 within two minutes
- (C) increases because of abdominal muscle fasciculations
- (D) increases because of an acetylcholine-like effect on the vagus nerve
- (E) peaks and subsides within five minutes
Which of the following complications of caudal anesthesia with 0.25% bupivacaine is more likely in children than in adults?
- (A) Intravascular injection
- (B) Neurotoxicity
- (C) Profound motor block
- (D) Systemic toxicity
- (E) Total spinal block
An 8-kg, 5-month-old infant undergoes craniotomy for an arteriovenous malformation. During the procedure, severe hemorrhaging occurs and packed red blood cells 3 units are transfused rapidly. During infusion of the third unit, hypotension, nodal bigeminy, and prolongation of the QT interval are noted. The most appropriate management includes administration of
- (A) bicarbonate
- (B) calcium
- (C) ephedrine
- (D) lidocaine
- (E) potassium
Which of the following statements concerning fetal hemoglobin is true?
- (A) It makes up less than 50% of the total hemoglobin in the neonate
- (B) It has less affinity for oxygen than adult hemoglobin
- (C) It binds with greater affinity to 2,3-DPG than adult hemoglobin
- (D) It shifts the oxyhemoglobin dissociation curve to the left
- (E) It has a P50 of 27 mmHg
During prolonged labor, a fetal scalp blood sample shows a PO2 of 21 mmHg, a PCO2 of 46 mmHg, and a pH of 7.35. These findings suggest
- (A) fetal hypoxemia
- (B) maternal hypoventilation
- (C) sampling of venous blood
- (D) miscalibration of the oxygen electrode
- (E) no abnormality
Which of the following is true of both the neonatal and adult airways?
- (A) Epiglottic innervation is primarily vagal
- (B) Sniffing position requires placement of a pillow under the occiput
- (C) The cricoid ring is the narrowest part of the airway
- (D) The epiglottis has a relatively similar size and shape
- (E) The glottis is located at C3-4
The most beneficial effect of continuous positive airway pressure in a newborn with respiratory distress syndrome is
- (A) increased functional residual capacity
- (B) decreased airway resistance
- (C) promotion of surfactant formation
- (D) increased alveolar PO2
- (E) maintenance of functional closure of the foramen ovale
The alveolar concentrations of anesthetics increase more rapidly in children than in adults because of a greater
- (A) blood volume (per kg body mass)
- (B) cardiac index
- (C) MAC
- (D) ratio of alveolar ventilation to functional residual capacity
- (E) tidal volume (per kg body mass)
A 1150-g, 10-day-old infant is undergoing a bowel resection for necrotizing enterocolitis. Heart rate is 200 bpm and blood pressure measured through a femoral artery catheter is 45/24 mmHg. The most appropriate next step is administration of
- (A) calcium gluconate
- (B) epinephrine
- (C) esmolol
- (D) fentanyl
- (E) normal saline solution
Thirty-six hours after primary repair of meningomyelocele, a term newborn has frequent periods of apnea lasting 25 seconds and associated with oxygen desaturation to 80%. The most likely explanation is
- (A) hyperglycemia
- (B) loss of cerebrospinal fluid
- (C) obstructive hydrocephalus
- (D) residual anesthetic effect
- (E) normal postoperative events
The rate of induction with inhalational agents is more rapid in neonates than adults because of a relatively increased
- (A) cardiac output
- (B) cerebral blood flow
- (C) functional residual capacity
- (D) metabolic rate
- (E) minute ventilation
After an uncomplicated cesarean delivery, a full-term neonate has intermittent cyanosis. Diaphragmatic effort is vigorous and respiratory distress is relieved while crying. The most likely diagnosis is
- (A) amniotic fluid aspiration
- (B) choanal atresia
- (C) diaphragmatic hernia
- (D) tetralogy of Fallot
- (E) tracheoesophageal fistula
A delay in surgery for 24 to 48 hours for preoperative stabilization and preparation is acceptable in each of the following neonatal conditions EXCEPT
- (A) biliary atresia
- (B) diaphragmatic hernia
- (C) meningomyelocele
- (D) pyloric stenosis
- (E) tracheoesophageal fistula
Nausea and vomiting in pediatric outpatients are
- (A) directly related to postoperative pain
- (B) unrelated to the length of the procedure
- (C) eliminated by preoperative administration of droperidol
- (D) eliminated by intraoperative nasogastric drainage
- (E) more frequent than in adults
Three hours prior to induction of anesthesia for elective laparotomy, a 40-kg 8-year-old boy is anxious and clings to his parents. Which of the following preanesthetic medications is most appropriate?
- (A) Oral ketamine
- (B) Oral midazolam
- (C) Rectal methohexital
- (D) Intramuscular droperidol
- (E) Intramuscular promethazine
An 8-kg, 1-year-old boy is scheduled for a bilateral inguinal hernia repair. If regional anesthesia is to be used for post-operative analgesia, which of the following statements is true?
- (A) Caudal administration of 0.25% bupivacaine will provide analgesia without evidence of motor block
- (B) Caudal administration of 0.125% bupivacaine is as effective as caudal administration of 0.25% bupivacaine
- (C) Caudal analgesia is more difficult to achieve in young children than in adults
- (D) The recommended volume of local anesthetic used for caudal analgesia in children is 3 ml per year of age
- (E) The volume of 0.25% bupivacaine required for bilateral ilioinguinal and iliohypogastric nerve blocks would be too large
A 4-month-old child undergoing a craniectomy for craniosynostosis is anesthetized with nitrous oxide and halothane. Suddenly the systolic blood pressure decreases from 75 to 30 mmHg, and the PetCO2 decreases from 35 to 6 mmHg. Which of the following maneuvers is LEAST likely to have a beneficial effect?
- (A) Administration of a fluid bolus
- (B) Administration of a vasopressor
- (C) Application of positive end-expiratory pressure
- (D) Discontinuation of nitrous oxide
- (E) Flooding the surgical wound with saline solution
Compared with adult hemoglobin, which of the following is a characteristic of fetal hemoglobin?
- (A) It has a greater oxygen-carrying capacity
- (B) It has a lower P50
- (C) It is more likely to cause an artifactual increase in Sp02
- (D) It is more likely to sickle
- (E) It unloads oxygen more readily at the tissues
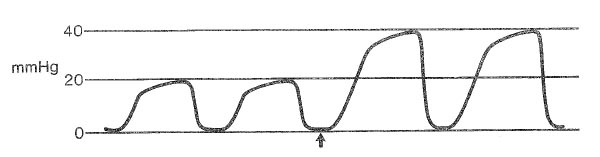
A 2-year-old child has cardiac arrest during an inguinal herniorrhaphy under general anesthesia administered during a Jackson-Rees system. The graph shows end-tidal PCO2 monitored from the tip of the endotracheal tube during cardiopulmonary resuscitation; minute ventilation is unchanged. Which of the following is the most likely cause of the change beginning at the arrow?
- (A) Decreased fresh gas flow
- (B) Inadequate chest compression
- (C) Increased dead space
- (D) Restoration of cardiac output
- (E) Sampling artifact
A 2500-g, 12-hour-old infant is tracheally intubated and mechanically ventilated at a rate of 20/min with an FiO2 of 0.4 and peak inspiratory pressure of 25 cmH2O. At birth, amniotic fluid was meconium stained and Apgar scores were 2 and 7. The most recent arterial blood gas levels are PaO2, 50 mmHg, PaCO2, 55 mmHg, and pH 7.20. The most appropriate management is to
- (A) administer sodium bicarbonate
- (B) begin intravenous infusion of prostaglandin E,
- (C) increase FiO2
- (D) increase ventilation
- (E) perform bronchial lavage
You are asked to evaluate a 2000-g male infant three hours after vaginal delivery because of a respiratory rate of 50/min, pulse rate of 115 bpm, and the following arterial blood gas values while breathing room air: PaO2 64 mmHg, PaCO2 43 mmHg, and pH 7.33. His mother received meperidine 75 mg two hours before delivery. Appropriate management includes
- (A) administration of naloxone 50 mcg intramuscularly
- (B) increasing the FiO2 to 0.4
- (C) intubation and mechanical ventilation at an FiO2 of 0.5
- (D) administration of oxygen 50% with 5 cm H2O continuous positive airway pressure
- (E) observation, with no action at present
A 2600-g neonate is to undergo surgical repair of a small gastroschisis. The infant is preoxygenated with 100% oxygen. Arterial hemoglobin desaturation is noted during laryngoscopy after a rapid-sequence induction. Which of the following is the most likely cause?
- (A) High fetal hemoglobin concentration
- (B) High ratio of oxygen consumption to functional residual capacity
- (C) Low functional residual capacity in milliliters per kilogram
- (D) Poor thoracic compliance
- (E) Patent ductus arteriosus
A 5-year-old child undergoes strabismus correction during spontaneous ventilation with halothane 1.5%, nitrous oxide and oxygen 50%. Intravenous atropine 0.2 mg is administered after inhalation induction. Ten minutes after incision, heart rate decreases from 110 bpm to 40 bpm. Which of the following is the most likely cause?
- (A) Administration of phenylephrine eyedrops
- (B) Inadvertent external pressure on the carotid sinus
- (C) Paradoxical response to a small dose of atropine
- (D) Sinoatrial nodal depression by halothane
- (E) Traction on an extraocular muscle
Infants with untreated pyloric stenosis are at increased risk for each of the following EXCEPT
- (A) congenital heart disease
- (B) dehydration
- (C) hypokalemia
- (D) increased gastric acidity
- (E) metabolic alkalosis
In an Infant, spinal anesthesia to a sensory level of T8 is achieved with tetracaine administered at the L2-3 interspace. Compared with spinal anesthesia to the same sensory level in an adult, this anesthetic is associated with a
- (A) higher risk for neurotoxicity
- (B) higher risk for systemic toxicity
- (C) lower risk for spinal cord injury
- (D) more significant decrease in blood pressure
- (E) shorter duration of action
A 6-year-old boy undergoes craniotomy in the supine position for brain tumor during anesthesia with 1.5% isoflurane in oxygen. PetCO2 is 38 mmHg, heart rate is 78 bpm, and blood pressure is 130/80 mmHg. After opening the dura, the surgeon notes that the brain is bulging. Which of the following management options is LEAST likely to significantly decrease brain size?
- (A) Decreased isoflurane concentration
- (B) Furosemide
- (C) Hyperventilation to a PaCO: of 25 mmHg
- (D) Mannitol
- (E) Nitroprusside
A parturient receives ketamine 2 mg/kg and succinylcholine 1.5 mg/kg for induction prior to elective cesarean delivery. Which of the following is most likely to be present in the newborn infant?
- (A) Normal muscle tone
- (B) Bradycardia
- (C) Opisthotonos
- (D) Respiratory depression
- (E) Seizures
A child has tachypnea immediately after reintubation for intractable laryngospasm. Oxygen saturation is 78% at an FiO2 of 1.0. A radiograph of the chest taken 15 minutes later is most likely to show
- (A) bilateral pleural effusions
- (B) diffuse homogenous pulmonary infiltrates
- (C) patchy central infiltrates of the right upper lobe
- (D) pneumothorax
- (E) segmental atelectasis at both lung bases
An 8-year-old child with chronic renal failure is scheduled for an operation to create an arteriovenous fistula. Laboratory studies include: Hemoglobin 6.5 g/dl, Blood gases (breathing air) : PaO2 97 mmHg, PaCO2 29 mmHg, pH 7.30 Sodium 129 mEq/L Potassium 5.5 mEq/L Chloride 101 mEq/L Bicarbonate 15 mEq/L. Before inducing general anesthesia, which of the following abnormalities should be corrected?
- (A) Anemia
- (B) Metabolic acidosis
- (C) Potassium concentration
- (D) Anemia, metabolic acidosis, and potassium concentration
- (E) None of the above
Which of the following is characteristic of the airway in a 2-month-oId infant when compared with an adult airway?
- (A) Airway is narrowest at the cricoid cartilage
- (B) Epiglottis is broader
- (C) Laryngeal mucosa is more tightly adherent
- (D) Larynx is positioned lower in the neck
- (E) Vocal cords have a more cephalad anterior attachment
A 5-month-old infant with tetralogy of Fallot is scheduled for elective inguinal herniorrhaphy. Which of the following would require the operation to be postponed?
- (A) Current propranolol therapy
- (B) Hematocrit of 65%
- (C) History of "tet spells"
- (D) Patent ductus arteriosus
- (E) Room air oxygen saturation of 82%
Inhalation induction of anesthesia is more rapid in a 6-month-old infant than in an adult because infants have
- (A) greater ratio of alveolar ventilation to functional residual capacity
- (B) greater ratio of blood volume to body weight
- (C) greater solubility of anesthetic in blood
- (D) lower anesthetic requirement
- (E) lower distribution of cardiac output to vessel-rich organs
Following maternal epidural injection, fetal exposure to chloroprocaine is lower than fetal exposure to bupivacaine for which of the following reasons?
- (A) Chloroprocaine is metabolized by plasma cholinesterase
- (B) Chloroprocaine is more protein bound
- (C) Chloroprocaine is not readily absorbed from the epidural space
- (D) The ionized fraction of chloroprocaine in the fetal circulation is smaller
- (E) The pKa of chloroprocaine is less than that of bupivacaine
The principal rationale for the use of warmed humidified inspired anesthetic gases in children is to
- (A) decrease postoperative respiratory complications
- (B) decrease postoperative shivering
- (C) preserve ciliary function
- (D) prevent dehydration
- (E) prevent evaporative heat loss
A 6-year-old child with severe cerebral palsy is scheduled for general anesthesia. He is at increased risk for each of the following EXCEPT
- (A) gastroesophageal reflux
- (B) hypersensitivity to central nervous system depressants
- (C) poor function of laryngeal reflexes
- (D) postoperative pulmonary complications
- (E) succinylcholine-induced hyperkalemia
A 5-year-old boy is to undergo microlaryngeal carbon dioxide laser vaporization of laryngotracheal papillomas under halothane administered through a small polyvinylchloride (PVC) endotracheal tube. The diluent gas mixture LEAST likely to support laser combustion of the PVC tube is
- (A) oxygen 40%, nitrous oxide 60%
- (B) oxygen 25%, nitrous oxide 75%
- (C) oxygen 30%, nitrogen 70%
- (D) oxygen 30%, helium 70%
- (E) oxygen 30%, air 70%
Compared with adults, neonates are more likely to become hypoxemic following anesthesia and extubation because of a relatively
- (A) higher rate of oxygen consumption
- (B) greater sensitivity to neuromuscular blockade
- (C) larger Vd/Vt ratio
- (D) lower blood pressure
- (E) smaller functional residual capacity
The MAC of a volatile anesthetic agent is greatest when administered to which of the following groups of healthy patients?
- (A) Neonates
- (B) Infants
- (C) Adolescents
- (D) Men 30 years of age
- (E) Parturients
An 18-month-old child with tetralogy of Fallot is anesthetized with halothane and nitrous oxide. Following intubation, oxygen saturation decreases abruptly from 85% to 45%. The most effective treatment is
- (A) discontinuation of halothane
- (B) hyperventilation
- (C) intravenous epinephrine
- (D) intravenous phenylephrine
- (E) positive end-expiratory pressure
During laser excision of vocal cord polyps in a 5-year-old boy, dark smoke suddenly appears in the surgical field. The trachea is intubated and anesthesia is being maintained with halothane, nitrous oxide, and oxygen. The most appropriate initial step is to
- (A) change from oxygen and nitrous oxide to air
- (B) fill the oropharynx with water
- (C) instill water into the endotracheal tube
- (D) remove the endotracheal tube
- (E) ventilate with carbon dioxide
A 2-year-old child is hospitalized for exposure. Rectal temperature is 30°C. The most appropriate method of warming is to
- (A) apply radiant heat
- (B) increase ambient temperature to 28°C
- (C) use a heating blanket set at 39°C
- (D) warm and humidify inspired gases
- (E) warm intravenous fluids to 37°C
A 20-kg, 6-year-old boy is undergoing strabismus surgery under anesthesia with sevoflurane, nitrous oxide, and oxygen. The heart rate suddenly decreases from 85 to 40 bpm. Which of the following is the most appropriate first step in management?
- (A) Decrease the depth of anesthesia
- (B) Increase the depth of anesthesia
- (C) Hyperventilate the patient
- (D) Administer atropine
- (E) Stop the surgical procedure
A full-term newborn has marked respiratory distress in the delivery room. Breath sounds are asymmetric and the abdomen is scaphoid. Which of the following maneuvers is most appropriate?
- (A) Hyperventilation with bag and mask
- (B) Intubation and ventilation with positive end-expiratory pressure
- (C) Intubation and ventilation with zero end-expiratory pressure
- (D) Bronchoscopy
- (E) Insertion of a chest tube
Which of the following would be most likely to result in neonatal depression when administered to a healthy parturient during an uncomplicated labor and vaginal delivery?
- (A) Nitrous oxide 60% in oxygen supplemented with halothane 0.5% for 10 minutes before delivery
- (B) Ketamine 20 mg intravenously 30 minutes before delivery
- (C) Meperidine 100 mg intramuscularly 2 hours before delivery
- (D) Thiopental 100 mg intravenously 30 minutes before delivery
- (E) Nitrous oxide 60% in oxygen supplemented with enflurane 0.7% for 10 minutes before delivery
Which of the following statements concerning caudal anesthesia in children is true?
- (A) The dural sac extends further caudad than in adults
- (B) Delay of postoperative micturition occurs in most patients
- (C) The sensory level of analgesia is poorly correlated with the dose of local anesthetic
- (D) It is technically difficult because of poorly defined sacral anatomy
- (E) It is contraindicated in infants younger than 1 year of age
Compared with a normal child, which of the following is expected during inhalation induction in a child with a 2:1 left-to-right intracardiac shunt?
- (A) Decreased rate of rise of alveolar anesthetic tension
- (B) Decreased anesthetic concentration in pulmonary artery blood
- (C) Decreased cerebral blood flow
- (D) Increased anesthetic concentration in vena cava blood
- (E) No difference in time for anesthetic induction
Which of the following findings is most likely in a 3-year-old child who has a secundum-type atrial septal defect with a 2:1 left-to-right shunt?
- (A) Pulmonary blood flow twice that of systemic blood flow
- (B) Pulmonary vascular resistance twice normal
- (C) Mean pulmonary artery pressure twice normal
- (D) Right atrial pressure twice normal
- (E) Hypoxemia while breathing room air
A meconium-stained, full-term infant has an initial Apgar score of 2. The oropharynx is suctioned and the infant is placed on a heated table. Which of the following is the most appropriate next step in management of the airway?
- (A) If the oropharynx is clear, observation for respiratory effort
- (B) Placement of an oxygen mask and application of positive pressure to clear the airway
- (C) Nasotracheal suctioning
- (D) Tracheal suctioning using the endotracheal tube
- (E) Intubation and ventilation with 100% oxygen
Which of the following conditions decreases right-to-left shunt through a patent ductus arteriosus in a neonate?
- (A) Arterial hypotension
- (B) Arterial hypoxemia
- (C) Metabolic acidemia
- (D) Positive end-expiratory pressure
- (E) Respiratory alkalemia
A 14-year-old girl with status asthmaticus is receiving oxygen 3 L/min through nasal prongs. Heart rate is 110 bpm. Arterial blood gas values are PaO2 90 mmHg, PaCO2 32 mmHg, and pH 7.46. If ventilation appears unchanged, which of the following is the most reliable sign of impending respiratory failure?
- (A) PaO2 of 80 mmHg
- (B) PaCO2 of 39 mmHg
- (C) Heart rate of 140 bpm
- (D) Increased wheezing
- (E) Deterioration of mental status
Which of the following is the primary physiologic response in a neonate exposed to a hypothermic environment?
- (A) Hyperventilation
- (B) Increased 2,3-DPG concentration in erythrocytes
- (C) Metabolism of brown fat
- (D) Shivering
- (E) Vasoconstriction
An infant becomes cyanotic and hypotensive after ventilatory pressures increase to 45 cm H2O during closure of the abdominal wall at the end of a gastroschisis repair. The most appropriate next step is to
- (A) administer a muscle relaxant
- (B) administer 5% dextrose in lactated Ringer's solution 10 ml/kg
- (C) change the endotracheal tube
- (D) ask the surgeon to insert a chest tube
- (E) ask the surgeon to reopen the abdomen
A 5-year-old child is brought to the emergency department in considerable respiratory distress. He is sitting leaning forward and drooling. He was well until four hours ago, when temperature increased to 38.9°C and he complained of a sore throat. The most appropriate initial management is to
- (A) administer nebulized racemic epinephrine
- (B) gently examine the airway with a tongue blade
- (C) obtain a lateral radiograph of the neck
- (D) perform a rapid induction-intubation sequence
- (E) perform inhalation induction without cricoid pressure
The newborn infant of an 18-year-old heroin addict has an initial Apgar score of 1. After intubation of the trachea and ventilation with pure oxygen, the Apgar score is 3 at five minutes. Appropriate management at this time would include administration of each of the following EXCEPT
- (A) dextrose 10%
- (B) epinephrine
- (C) naloxone
- (D) normal saline solution
- (E) sodium bicarbonate
A 7-year-old, obese, 30-kg boy was anesthetized using an adult circle system containing a 3-liter bag and mask. Induction with nitrous oxide (2 liters), oxygen (1 liter), and enflurane 3% was characterized by three minutes of hyperventilation followed by apnea. Forty-five seconds later, the child moved and became difficult to control. The most likely cause of the movement is
- (A) decreased alveolar concentration of enflurane during the period of apnea
- (B) excessive uptake of enflurane by the child's fat
- (C) higher fresh gas flows required with use of an adult circle system in a child
- (D) convulsions induced by enflurane
- (E) hypoxia developing during the period of apnea
An otherwise healthy 16-year-old girl is undergoing posterior spinal fusion for thoracolumbar scoliosis. During the procedure, the most likely cause of a marked decrease in the amplitude of the somatosensory evoked potentials after stimulation of the posterior tibial nerve is
- (A) administration of fentanyl 30 jag /kg for induction
- (B) administration of isoflurane 1.3 MAC for maintenance
- (C) administration of vecuronium 0.15 mg/kg
- (D) a decrease in body temperature from 37 to 35°C
- (E) a decrease in cerebrospinal fluid pressure
A 15-kg, 3-year-old child is anesthetized for an inguinal hernia repair with halothane and nitrous oxide. The trachea is intubated after administration of succinylcholine 30 mg. At the conclusion of the 45-minute procedure, the child is not breathing; a peripheral nerve twitch monitor indicates no response to a train-of-four stimulus. Further investigation is most likely to show
- (A) abnormal response to nondepolarizing muscle relaxants
- (B) a low dibucaine number
- (C) a low plasma cholinesterase concentration
- (D) an underlying myopathy
- (E) a positive halothane-caffeine contracture test
A 4-year-old child has just undergone a one-hour tonsillectomy with a volatile anesthetic, nitrous oxide, and oxygen. Which of the following will result in the most rapid emergence?
- (A) Decreased PaCO2
- (B) Increased cardiac output
- (C) Increased fresh gas flow
- (D) Increased solubility of the volatile agent
- (E) Presence of a ventricular septal defect
A newborn infant is undergoing repair of gastroschisis. During closure of the abdominal wall, ventilatory pressures and central venous pressure increase markedly. The most appropriate management is to
- (A) administer a bronchodilator
- (B) decrease tidal volume and increase ventilatory rate
- (C) increase the neuromuscular block
- (D) increase the depth of anesthesia
- (E) ask the surgeon to reopen the abdomen
An 8-kg, 1-year-old child has a measured blood loss of 50 ml during the first two hours of a rectal pull-through operation. Preoperative hematocrit was 31%. Balanced saline solution 150 ml has been administered for replacement. Urine output has been 2 ml for the last hour, heart rate is 160 bpm, and blood pressure is 40/15 mmHg. The most appropriate fluid therapy is,
- (A) 25% albumin
- (B) balanced salt solution
- (C) balanced salt solution and mannitol
- (D) 5% dextrose in 0.45% saline solution
- (E) packed red blood cells
Which of the following statements concerning the retinopathy of prematurity is true?
- (A) The initial lesion is dilation of retinal capillaries
- (B) It can be prevented by maintaining FiO2 below 0.4
- (C) It is less likely to develop if PaO2 is maintained below 70 mmHg
- (D) The incidence is unrelated to birth weight
- (E) Infants whose postconceptual age has reached 40 weeks are no longer at risk
A 14-month-old child has tetralogy of Fallot with dynamic obstruction to right ventricular outflow. Which of the following is most likely to decrease cyanosis in this child?
- (A) Calcium
- (B) Epinephrine
- (C) Nitroglycerin
- (D) Nitroprusside
- (E) Propranolol
A 20-kg, 5-year-old boy under treatment for five days for a cerebral contusion not requiring an operation is still unconscious. After three days of mechanical ventilation, humidified oxygen 40% via T-tube is started. Arterial blood gas analysis shows PaO2 120 mmHg, PaCO2 44 mmHg, pH 7.48, and base excess +6. A nasogastric tube is in place and draining to gravity. Daily fluid therapy has been 5% dextrose in 0.5 normal saline solution 500 ml and 5% dextrose in lactated Ringer's solution 500 ml. Serum electrolyte concentrations are sodium 140, potassium 3.2, and chloride 91 mEq/L. Serum osmolality is 300 mOsm/L. Urine output averages 15 ml/hour. Dexamethasone 8 mg/day has been the only drug therapy. This patient most likely requires
- (A) additional intravenous fluids
- (B) furosemide diuresis
- (C) administration of ammonium chloride
- (D) reinstitution of mechanical ventilation
- (E) administration of potassium chloride
A 1-month-old infant becomes hypoxemic faster during apnea than an adult. Which of the following is the primary cause of this difference?
- (A) Functional residual capacity in an infant is half that of an adult
- (B) Metabolic rate in an infant is twice that of an adult
- (C) Resting PaO2 in an infant is lower than that in an adult
- (D) The number of alveoli in an infant is 12% the number in an adult
- (E) The hemoglobin dissociation curve in an infant is shifted to the right
During an inguinal hernia repair, a newborn infant will have a larger fluid requirement (in milliliters per kilogram) than an adult because of relatively greater
- (A) insensible water loss
- (B) lean body mass
- (C) metabolic rate
- (D) sodium loss
- (E) third space losses
The most important anesthetic consideration in Pierre Robin syndrome is
- (A) anterior tilt of the larynx
- (B) hyperplasia of the internal surface of the maxilla
- (C) mandibular hypoplasia
- (D) hypertrophy of the epiglottis
- (E) tracheomalacia
Which of the following statements regarding fetal heart rate patterns is true?
- (A) Early decelerations suggest umbilical cord compression
- (B) Fetal heart rates between 160 and 180 bpm are normal
- (C) Fetal heart rate unaffected by uterine contraction suggests fetal well-being
- (D) Late decelerations indicate inadequate uteroplacental perfusion
- (E) Variable decelerations indicate need for urgent delivery
The most effective treatment of severe carbon monoxide poisoning in a 2-year-old child is
- (A) intravenous administration of methylene blue
- (B) intravenous administration of thiocyanate
- (C) intravenous administration of thiosulfate
- (D) exchange transfusion
- (E) hyperbaric oxygenation
Which the following findings is most hazardous in premature infants?
- (A) Hematocrit of 55%
- (B) Rectal temperature of 35 degrees C
- (C) Umbilical arterial blood PO2 of 50 mmHg
- (D) Umbilical arterial blood PCO2 of 45 mmHg
- (E) Umbilical arterial systolic pressure of 60 mmHg
Optimal ventilation of a newborn with congenital diaphragmatic hernia should consist of
- (A) PaCO2 30 mmHg, low tidal volumes
- (B) PaCO2 30 mmHg, high tidal volumes
- (C) PaCO2 40 mmHg, low tidal volumes
- (D) PaCO2 40 mmHg, high tidal volumes
- (E) PaCO2 45 mmHg, low tidal volumes
A 10-week-old infant born at 28 weeks gestation is scheduled for elective repair of bilateral inguinal hernias. It is most appropriate to
- (A) delay the operation until the infant is 6 months old
- (B) transfuse blood preoperatively if hemoglobin concentration is 9 g/dl
- (C) avoid tracheal intubation
- (D) limit inspired oxygen concentration to less than 50%
- (E) monitor for apnea for 24 hours postoperatively
An infant is delivered by forceps following labor in which variable decelerations were noted. Amniotic fluid was clear. Initial evaluation shows a cyanotic, limp infant with a heart rate of 80 bpm, poor respiratory efforts, and grimacing in response to suctioning. The most appropriate method of resuscitation for this newborn is
- (A) vigorous tactile stimulation
- (B) bag and mask ventilation with oxygen
- (C) immediate endotracheal intubation
- (D) administration of sodium bicarbonate 1 mEq/kg
- (E) volume expansion with normal saline solution 10 mL/kg
A 1100-g, 10-day-old infant is to undergo ligation of a patent ductus arteriosus after unsuccessful medical treatment. Within three minutes of intravenous administration of atropine 20 mcg, fentanyl 20 mcg, and pancuronium 0.1 mg, systemic blood pressure decreases from 80 to 30 mmHg, heart rate from 180 to 140 bpm, and arterial oxygen saturation from 90% to 80%. The most appropriate management is to
- (A) increase FiO2
- (B) administer additional atropine
- (C) infuse crystalloid
- (D) infuse prostaglandin E1
- (E) administer phenylephrine
Which of the following is suggestive of epiglottitis rather than croup?
- (A) A 2-year-old child with a harsh, barking cough
- (B) A 4-year-old child who insists on sitting up and leaning forward
- (C) Leukocyte count of 10,000/mm3 with marked lymphocytosis
- (D) Rectal temperature of 38.5°C
- (E) Subglottic narrowing (steeple sign) on lateral neck radiograph
A 2.2-kg, 6-hour-old neonate is to undergo gastrostomy followed by repair of a tracheoesophageal fistula. During induction with halothane, air, and oxygen, the abdomen becomes distended. Appropriate management is to
- (A) intubate and assist spontaneous ventilation
- (B) intubate and control ventilation
- (C) insert an orogastric tube
- (D) allow the patient to breathe spontaneously by mask until gastrostomy
- (E) control ventilation by mask until gastrostomy
In a 5-kg boy with Treacher Collins syndrome who is to undergo cleft palate repair, endotracheal intubation is best accomplished with
- (A) awake nasal intubation after topical anesthesia
- (B) halothane anesthesia with spontaneous ventilation
- (C) light isoflurane anesthesia and a muscle relaxant
- (D) thiopental and succinylcholine sequence intravenously
- (E) nasal intubation after administration of ketamine intramuscularly
A newborn is in respiratory distress. Examination shows a scaphoid abdomen, cyanosis while breathing oxygen by mask, and heart sounds in the right hemithorax. Which of the following is the most appropriate next step?
- (A) Assisted ventilation with a bag and face mask
- (B) Insertion of a chest tube on the left side
- (C) Insertion of a nasogastric tube
- (D) Tracheal intubation and assisted ventilation
- (E) Tracheal intubation and expansion of the left lung
A full-term neonate has physical findings suggestive of congenital diaphragmatic hernia. Initial Apgar score is 2. Which of the following is the most appropriate initial management?
- (A) Placement of an orogastric tube
- (B) Insertion of a chest tube
- (C) Controlled ventilation by face mask
- (D) Controlled ventilation through an endotracheal tube
- (E) Spontaneous ventilation through an endotracheal tube
Which of the following results in the greatest increase in right-to-left shunting in an infant with cyanotic heart disease?
- (A) Decreased pulmonary vascular resistance
- (B) Decreased systemic vascular resistance
- (C) Hemodilution
- (D) Increased heart rate
- (E) Myocardial depression
The portion of the infant airway with the smallest cross-sectional area occurs at the level of the
- (A) cricoid cartilage
- (B) false vocal cords
- (C) thoracic inlet
- (D) tonsillar pillars
- (E) true vocal cords
The adult oxyhemoglobin dissociation curve will resemble that of the fetus in the presence of
- (A) increased 2,3-diphosphoglycerate concentration
- (B) chronic anemia
- (C) hyperthermia
- (D) metabolic alkalemia
- (E) hyperkalemia
An infant with congenital lobar emphysema is scheduled for thoracotomy. Which of the following should be included in the anesthetic management of this infant?
- (A) Helium-oxygen inspired gas mixture
- (B) Nitrous oxide administration
- (C) Positive pressure ventilation
- (D) Prophylactic placement of a chest tube
- (E) Spontaneous ventilation until the chest is opened
Which of the following is an effect of hypothermia in neonates?
- (A) Decreased duration of neuromuscular blockade
- (B) Increased narcotic requirements
- (C) Increased pulmonary vascular resistance
- (D) Metabolic alkalosis
- (E) Shivering
A 35-kg child requires mechanical ventilation with 100% oxygen at a tidal volume of 350 mL and a rate of 20/min during a severe asthma attack. The most likely cause of severe hypotension after initiating mechanical ventilation is
- (A) hypoxic circulatory depression
- (B) inadequate expiratory time
- (C) increased pulmonary vascular resistance
- (D) respiratory alkalosis
- (E) tension pneumothorax
A 3-day-old infant is comatose 18 hours after surgical correction of transposition of the great vessels. Tracheal suctioning produces only a tachycardic response. Anesthesia included midazolam 0.5 mg/kg, fentanyl 60 mcg/kg, and pancuronium 0.3 mg/kg. Which of the following is the most appropriate first step in evaluation of this infant?
- (A) Administration of flumazenil
- (B) Administration of naloxone
- (C) Train-of-four assessment
- (D) CT scan of the head
- (E) EEG
Acute epiglottitis usually
- (A) requires a lateral radiograph of the neck for diagnosis
- (B) occurs in children 2 to 4 years of age
- (C) is treated effectively with racemic epinephrine
- (D) has a viral etiology
- (E) requires immediate awake intubation by direct laryngoscopy in the emergency department
During Harrington rod instrumentation for scoliosis, monitoring somatosensory evoked potentials
- (A) is unreliable if halothane is used
- (B) eliminates the need for a wake-up test
- (C) accurately assesses proprioceptive integrity
- (D) accurately assesses motor function integrity
- (E) is unreliable if nondepolarizing muscle relaxants are used
A 22-year-old woman with severe preeclampsia vaginally delivers a 3-kg infant after 12 hours of treatment with magnesium sulfate and continuous epidural infusion of bupivacaine 0.0625% and fentanyl 1 mcg/ml at 10 ml/hr. The infant is pink and hypotonic; heart rate is 110 bpm and blood pressure is 35/25 mmHg. Which of the following is the most appropriate initial management of the infant?
- (A) 10% Dextrose in water
- (B) Calcium gluconate
- (C) Epinephrine
- (D) Naloxone
- (E) Intubation and ventilation
Which of the following should be included in the preoperative management of a 12-year-old patient with Duchenne's muscular dystrophy who is unable to ambulate?
- (A) Determination of serum creatine kinase concentration
- (B) Determination of serum potassium concentration
- (C) Liver function profile
- (D) Echocardiography
- (E) Dantrolene prophylaxis
A 4-year-old child with myelomeningocele and a ventriculoperitoneal shunt is scheduled for bladder augmentation. One year ago, hypotension and bronchospasm occurred during laparotomy for placement of a feeding gastrostomy and responded to fluids and epinephrine. At that time, anesthesia was induced with thiopental, the trachea was intubated with a polyvinyl tracheal tube following administration of succinylcholine, and anesthesia was maintained with halothane and nitrous oxide. No diagnostic tests were performed after that incident. Which of the following should be avoided during the bladder augmentation?
- (A) Latex gloves
- (B) Polyvinyl tracheal tubes
- (C) Halothane
- (D) Succinylcholine
- (E) Thiopental
At the time of cesarean delivery, thick dark meconium is noted and the newborn is flaccid, apneic, bradycardic, and cyanotic. The most appropriate initial action is
- (A) atropine administration
- (B) sodium bicarbonate administration
- (C) naloxone administration
- (D) controlled ventilation
- (E) tracheal suctioning
Which of the following statements concerning cardiovascular physiology in a healthy term neonate is true?
- (A) Heart rate is increased in response to hypoxemia
- (B) Heart rate increases reflexly in response to hypotension
- (C) Stroke volume increases in response to decreased systemic vascular resistance
- (D) Stroke volume increases in response to bradycardia
- (E) Stroke volume is near-maximal under resting conditions
Each of the following is a characteristic of prostaglandin E1 (alprostadil) pharmacology in an infant EXCEPT:
- (A) It is effective in the treatment of large left-to-right shunts
- (B) It is a cause of apnea
- (C) It is a potent vasodilator
- (D) It prevents closure of the ductus arteriosus
- (E) It is metabolized rapidly
A child undergoing general anesthesia is breathing spontaneously using the Jackson-Rees modification of the Ayres T-piece. Respiratory rate is 20/min and tidal volume is 75 ml. What is the minimum fresh gas flow required to prevent rebreathing?
- (A) 750 ml/min
- (B) 1500 ml/min
- (C) 2250 ml/min
- (D) 4500 ml/min
- (E) 6000 ml/min
A healthy 10-kg child is flushed and restless after premedication with meperidine 15 mg and scopolamine 0.2 mg intramuscularly. His skin is warm and dry; temperature is 38°C, pulse is 130 bpm, and blood pressure is 90/60 mmHg. The most likely cause is
- (A) dehydration
- (B) idiosyncratic reaction to meperidine
- (C) malignant hyperthermia
- (D) neuroleptic malignant syndrome
- (E) scopolamine
Compared with adults, neonatal respiratory function is characterized by
- (A) a lower ratio of dead space to tidal volume
- (B) a more compliant chest wall
- (C) a more positive intrapleural pressure at end-expiration
- (D) less susceptibility to atelectasis
- (E) the same oxygen requirement per kilogram of body weight
A 2.8-kg 8-hour-old infant undergoes laparotomy for a ruptured omphalocele. Following primary closure of the abdominal wall, arterial blood gases are PaO2 40 mmHg (FiO2 0.6), PaCO2 55 mmHg, and pH 7.1. Blood pressure is 30/20 mmHg. After increasing the FiO2, the most appropriate action would be to
- (A) obtain a radiograph of the chest immediately
- (B) withdraw the endotracheal tube 1 cm
- (C) assess the patient for coexisting congenital heart disease
- (D) administer lactated Ringer's solution 15 ml/kg
- (E) ask the surgeon to reopen the wound
In an infant, spinal anesthesia to a sensory level of T8 is achieved with tetracaine administered at the L2-3 interspace. Compared with spinal anesthesia to the same sensory level in an adult, this anesthetic is associated with a
- (A) greater decrease in blood pressure
- (B) higher risk for neurotoxicity
- (C) higher risk for systemic toxicity
- (D) lower risk for spinal cord injury
- (E) shorter duration of action
In a 5-kg child, the end-tidal carbon dioxide tension is 35 mmHg during spontaneous ventilation through a Mapleson D system. Which single change is most likely to increase this value?
- (A) Decreasing the fresh gas flow
- (B) Increasing respiratory minute volume
- (C) Opening the pressure release valve
- (D) Removing the reservoir bag
- (E) Substituting larger bore tubing
During uncomplicated mask induction with halothane and 50% nitrous oxide in oxygen in a 6-month-old infant with a large ventricular septal defect and valvular pulmonic stenosis, SpO2 decreases from 85% (room air) to 60%; heart rate is 100 bpm and blood pressure is 62/40 mmHg. The most appropriate management is to
- (A) administer atropine
- (B) administer phenylephrine
- (C) administer propranolol
- (D) increase anesthetic depth
- (E) intubate the trachea
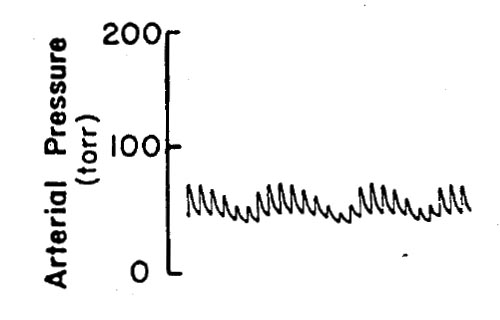
A mechanically ventilated newborn infant is undergoing gastroschisis repair during halothane anesthesia. Based on the right radial artery catheter tracing shown, which of the following is the most appropriate conclusion?
- (A) The abdomen has not yet been incised
- (B) The anesthetic should be changed from halothane to isoflurane
- (C) The ductus arteriosus is still open
- (D) The infant is hypovolemic
- (E) The tidal volume is inadequate
A 2.3-kg 1-day-old term infant requires repair of a gastroschisis. Which of the following combinations is most appropriate for intraoperative fluid management?
- (A) Dextrose 5% in water for maintenance and lactated Ringer's solution for replacement of third space losses
- (B) Dextrose 10% in water for maintenance and lactated Ringer's solution for replacement of third space losses
- (C) Lactated Ringer's solution for maintenance and replacement of third space losses
- (D) Lactated Ringer's solution for maintenance and albumin 5% for replacement of third space losses
- (E) Normal saline solution for maintenance and lactated Ringer's solution for replacement of third space losses
Which of the following features is characteristic of the airway in a neonate?
- (A) Glottis that is located at the level of the C6 vertebral body
- (B) Larger tongue relative to the head than in an adult
- (C) Laryngeal mucosa that is densely adherent to the cartilages
- (D) More posterior glottis than that of an adult
- (E) Narrowest portion of the airway that is located at the arytenoid cartilages
Compared with adults, neonates are more likely to become hypoxemic following anesthesia and extubation because of a relatively
- (A) higher rate of oxygen consumption
- (B) greater sensitivity to neuromuscular blockade
- (C) larger Vd/Vt ratio
- (D) lower blood pressure
- (E) smaller functional residual capacity
Anesthesia is induced with halothane in a 3-year-old girl. Sixty seconds after administration of succinylcholine 1 mg/kg intravenously, heart rate decreases rapidly from 120 to 60 bpm. The most likely cause is
- (A) acute hyperkalemia
- (B) failure to pretreat with a nondepolarizing relaxant
- (C) halothane overdose
- (D) muscarinic activity
- (E) sympathetic ganglionic blockade
Compared with similar use in adults, routine use of succinylcholine in children is hazardous because of the increased risk for which of the following?
- (A) Anaphylactoid reaction
- (B) Phase II blockade
- (C) Pseudocholinesterase deficiency
- (D) Pulmonary aspiration
- (E) Undiagnosed myopathy
A 3.3-kg neonate is brought to the operating room for repair of a left diaphragmatic hernia. A 3-mm endotracheal tube is placed to a depth of 9 cm. Initial arterial blood gas values from a right radial catheter while spontaneously breathing oxygen 50% are PaO2 82 mmHg, PaCO2 41 mmHg, pH 7.33, and base excess -5. After reduction of the hernia (during closure of the abdomen), vigorous attempts to expand the atelectatic lung are unsuccessful. The infant rapidly becomes very dusky, heart rate is 60 bpm, breath sounds are distant and squeaky bilaterally, and pulmonary compliance is decreased. Which of the following should be done first?
- (A) Obtain a radiograph of the chest
- (B) Place a chest tube on the left side
- (C) Place a chest tube on the right side
- (D) Withdraw the endotracheal tube 1 cm and suction
- (E) Reopen the abdomen
Which of the following should be included in the preoperative management of a 12-year-old patient with Duchenne muscular dystrophy who is unable to ambulate?
- (A) Determination of serum creatine kinase concentration
- (B) Determination of serum potassium concentration
- (C) Liver function profile
- (D) Echocardiography
- (E) Dantrolene prophylaxis
Which of the following parts of the infant's airway determines the appropriate diameter of a nasotracheal tube?
- (A) Nares
- (B) Glottis
- (C) Vocal cords
- (D) Cricoid cartilage
- (E) Third tracheal ring
In calculating the fluid requirements for a newborn undergoing repair of an omphalocele, the third-space loss should be replaced by
- (A) 0.9% saline solution
- (B) 2.5% dextrose in 0.45% saline solution
- (C) 5% dextrose in lactated Ringer's solution
- (D) 5% dextrose in water
- (E) 5% dextrose in 0.25% saline solution
Compared with adults, caudal anesthesia in children is associated with
- (A) higher risk for subarachnoid puncture
- (B) more severe hypotension
- (C) more rapid onset of sensory block
- (D) smaller volume of anesthetic per kilogram of body weight
- (E) toxic effects at lower serum levels of bupivacaine
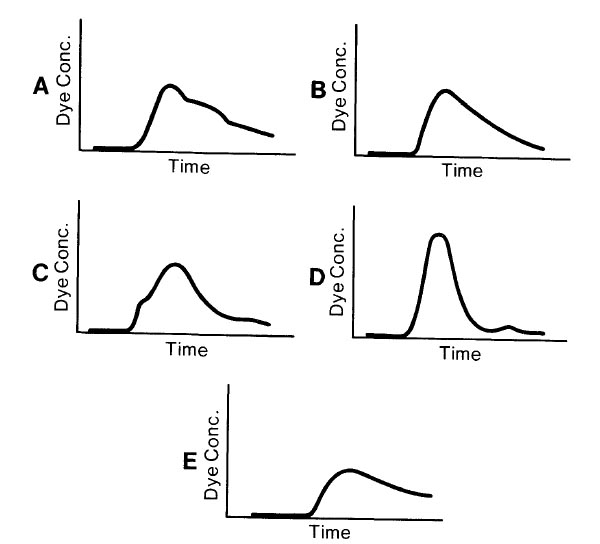
Which of the following time concentration curves would be expected in arterial blood following intravenous injection of indocyanine green dye in a 3-year-old child with a small ventricular septal defect?
Compared with normal adults, which of the following characteristics of neonates best explains the more rapid inhalation induction in neonates?
- (A) Greater cardiac index
- (B) Greater metabolic rate
- (C) Greater perfusion of vessel-rich tissues
- (D) Greater ratio of alveolar ventilation to functional residual capacity
- (E) Less lean body mass
In children with preoperative upper respiratory tract infection, which of the following is associated with the greatest risk for postoperative airway obstruction?
- (A) Age less than 1 year
- (B) Endotracheal intubation
- (C) Head and neck surgery
- (D) Inadequate airway humidification
- (E) Surgery for more than two hours
Which of the following best explains why neonates are at greater risk than adults for hypothermia during surgical procedures?
- (A) Greater body surface area relative to body mass
- (B) Greater cutaneous vasodilation at equal MAC concentrations of volatile anesthetics
- (C) Greater dependence on shivering to produce heat
- (D) Inability to increase metabolic rate
- (E) Less insulation by adipose tissue
A 60-kg, 17-year-old girl with severe idiopathic scoliosis is scheduled for Harrington rod fixation. Which of the following respiratory parameters is compatible with this disorder?
- (A) Alveolar-to-arterial oxygen tension difference (A-aDO2) less than 100 mmHg while breathing pure oxygen
- (B) FEV1/FVC ratio less than 50%
- (C) Forced vital capacity less than 2000 ml
- (D) Intrapulmonary shunt less than 10%
- (E) Normal pulmonary vascular resistance
A 2.8-kg newborn undergoes repair of a moderate-sized omphalocele. Intravenous fluid is administered at 14 mL/hr. Forty-five minutes after beginning surgery and before reduction of the omphalocele, arterial blood pressure decreases from 80/40 to 55/30 mmHg. SaO2 is 98% at an FiO2 of 0.5. Breath sounds are equal bilaterally. Which of the following is the most likely explanation for the decrease in blood pressure?
- (A) Associated congenital cardiac defect
- (B) Compression of the lungs by the abdominal contents
- (C) Inadequate fluid administration
- (D) Pneumothorax
- (E) Sepsis
During ligation of a patent ductus arteriosus, a newborn infant receives a total gas flow of 5 L/min through a nonheated Jackson-Rees system. Operating room temperature is maintained at 30°C. The primary cause of a rapid decrease in rectal temperature from 36.8°C to 35°C is
- (A) absence of the central temperature control mechanism
- (B) conductive heat loss
- (C) convective heat loss
- (D) evaporative heat loss
- (E) radiant heat loss
Compared with the adult airway, the neonatal airway has which of the following characteristics?
- (A) More cephalad larynx
- (B) Narrowest diameter at the vocal cords
- (C) Relatively smaller epiglottis
- (D) Smaller tongue relative to the size of the oral cavity
- (E) Vocal cords perpendicular to the trachea
A 6-year-old child with asthma begins wheezing during anesthesia with halothane and nitrous oxide in oxygen. A loading dose of aminophylline is administered followed by continuous infusion. Premature ventricular contractions appear on the ECG. The most appropriate management is to
- (A) administer fentanyl
- (B) discontinue aminophylline
- (C) increase exhalation time
- (D) increase the inspired concentration of halothane
- (E) switch the inhalational agent to isoflurane
Compared with the adult airway, the airway of an infant is characterized by
- (A) greater narrowing at the cricoid ring
- (B) a less rigid epiglottis
- (C) a more caudad laryngeal opening
- (D) a relatively smaller tongue
- (E) relatively larger tonsils