56 questions match your search.
Five minutes after initiating one-lung ventilation using a double-lumen endobronchial tube, a 70-year-old patient has a decrease in Sp02 from 99% to 90%. Tidal volume and respiratory rate are unchanged. Fiberoptic bronchoscopy verifies appropriate positioning of the tube. Which of the following is the most likely cause of the desaturation?
- (A) Blood flow to the nondependent lung
- (B) Failure of hypoxic pulmonary vasoconstriction in the dependent lung
- (C) Inadequate filling of the bronchial cuff
- (D) Inadequate minute ventilation
- (E) Surgical manipulation of the nondependent lung
A woman with chronic obstructive pulmonary disease is extubated and minimally responsive after isoflurane anesthesia. She is receiving oxygen 6 L/min through a face mask. Respirations are 10/min, PaO2 is 68 mmHg, PaCO2 is 54 mmHg, and pH is 7.28. The most likely cause of the respiratory acidemia is
- (A) blunted sensitivity to low pH in the medullary respiratory center
- (B) chronic carbon dioxide retention
- (C) decreased lung volume from supine positioning
- (D) depression of carotid body chemoreceptors by halothane
- (E) suppression of hypoxic ventilatory drive by supplemental oxygen
A 50-year-old man who takes aspirin and nifedipine is scheduled for thoracotomy with one-lung ventilation. Which of the following is associated with the greatest risk for intraoperative hypoxemia?
- (A) Preoperative withdrawal of nifedipine therapy
- (B) Intraoperative mild respiratory acidosis
- (C) Intraoperative administration of isoflurane
- (D) Intraoperative administration of nitroglycerin
- (E) Intraoperative thoracic epidural morphine
A patient is undergoing thoracotomy in the lateral position. Five minutes after initiation of one-lung ventilation using a double-lumen tube and 100% oxygen, SpO2 decreases from 100% to 65%. Which of the following is the most appropriate initial step in management?
- (A) Adding continuous positive airway pressure to the nondependent lung
- (B) Adding positive end-expiratory pressure to the dependent lung
- (C) Increasing the tidal volume to the dependent lung
- (D) Resuming two-lung ventilation
- (E) Verifying the position of the double-lumen tube
After the bronchial and tracheal cuffs of a right endobronchial tube are inflated, ventilation through the tracheal lumen is not possible. This finding is most consistent with
- (A) cuff occlusion of the right upper lobe bronchus
- (B) intubation of the left bronchus
- (C) left-sided tension pneumothorax
- (D) overinflation of the bronchial cuff
- (E) positioning of both cuffs in the trachea
During induction of general anesthesia in a patient with a supraglottic tumor, both intubation and subsequent ventilation via a face mask are impossible. A cricothyroidotomy is performed with a 16-gauge intravenous catheter. Which of the following statements is true?
- (A) Application of pressures greater than 35 cmH2O to the catheter will increase the risk for pulmonary barotrauma
- (B) PaC02 can be maintained at a normal level using a standard circle system attached to the catheter
- (C) PaO2 greater than 100 mmHg can be maintained indefinitely using transtracheal jet ventilation with pure oxygen through the catheter
- (D) Emergency surgical tracheostomy would have improved the likelihood of survival
- (E) The presence of this tumor contraindicates jet ventilation via cricothyroidotomy
Prior to occlusion of any major pulmonary blood vessels during a thoracotomy, applying positive end-expiratory pressure to ventilation through the dependent lumen of a double-lumen tube and occluding the upper lumen of the tube will
- (A) increase blood flow to the dependent lung
- (B) increase the alveolar-arterial oxygen tension difference
- (C) override hypercarbic pulmonary vasoconstriction
- (D) improve the patient's oxygenation
- (E) increase the right ventricular dP/dt
Compared with a person of normal weight, which of the following findings are most likely on pulmonary function testing of a patient with morbid obesity? (FVC, FEV/FVC, FRC, A-a DO2)?
- (A) Decreased, Normal, Decreased, Normal
- (B) Decreased, Normal, Decreased , Increased
- (C) Decreased, Normal, Normal, Increased,
- (D) Increased, Decreased, Normal, Increased
- (E) Increased, Decreased, Decreased, Increased
A 35-year-old woman with severe myasthenia gravis is scheduled for thymectomy. Which of the following preoperative pulmonary function tests is most likely to be normal?
- (A) Forced expiratory volume in 1 second (FEV1)
- (B) Forced vital capacity (FVC)
- (C) FEV1/FVC
- (D) Maximum voluntary ventilation
- (E) Peak inspiratory force
An 8-year-old child with chronic renal failure is scheduled for an operation to create an arteriovenous fistula. Laboratory studies include: Hemoglobin 6.5 g/dl, Blood gases (breathing air) : PaO2 97 mmHg, PaCO2 29 mmHg, pH 7.30 Sodium 129 mEq/L Potassium 5.5 mEq/L Chloride 101 mEq/L Bicarbonate 15 mEq/L. Before inducing general anesthesia, which of the following abnormalities should be corrected?
- (A) Anemia
- (B) Metabolic acidosis
- (C) Potassium concentration
- (D) Anemia, metabolic acidosis, and potassium concentration
- (E) None of the above
A child has tachypnea immediately after reintubation for intractable laryngospasm. Oxygen saturation is 78% at an FiO2 of 1.0. A radiograph of the chest taken 15 minutes later is most likely to show
- (A) bilateral pleural effusions
- (B) diffuse homogenous pulmonary infiltrates
- (C) patchy central infiltrates of the right upper lobe
- (D) pneumothorax
- (E) segmental atelectasis at both lung bases
Which of the following statements regarding carbon monoxide poisoning is true?
- (A) Breathing 100% oxygen at 1 atmosphere reduces the carboxyhemoglobin half-life
- (B) Effective treatment includes administration of methylene blue
- (C) It is commonly associated with respiratory acidosis
- (D) It is incompatible with a normal Sp02 while breathing room air
- (E) The oxyhemoglobin dissociation curve is shifted to the right
An acutely ill 65-year-old man with sepsis has severe hypophosphatemia. Which of the following is most likely to result from this electrolyte disorder?
- (A) Bronchospasm
- (B) Diarrhea
- (C) Muscle weakness
- (D) Seizures
- (E) Ventricular ectopy
A 20-kg, 5-year-old boy under treatment for five days for a cerebral contusion not requiring an operation is still unconscious. After three days of mechanical ventilation, humidified oxygen 40% via T-tube is started. Arterial blood gas analysis shows PaO2 120 mmHg, PaCO2 44 mmHg, pH 7.48, and base excess +6. A nasogastric tube is in place and draining to gravity. Daily fluid therapy has been 5% dextrose in 0.5 normal saline solution 500 ml and 5% dextrose in lactated Ringer's solution 500 ml. Serum electrolyte concentrations are sodium 140, potassium 3.2, and chloride 91 mEq/L. Serum osmolality is 300 mOsm/L. Urine output averages 15 ml/hour. Dexamethasone 8 mg/day has been the only drug therapy. This patient most likely requires
- (A) additional intravenous fluids
- (B) furosemide diuresis
- (C) administration of ammonium chloride
- (D) reinstitution of mechanical ventilation
- (E) administration of potassium chloride
In a 65-year-old man, which of the following findings on preoperative pulmonary function testing is associated with the highest risk for respiratory insufficiency following pneumonectomy?
- (A) Maximum voluntary ventilation at 65% of predicted
- (B) Mean pulmonary artery pressure of 28 mmHg
- (C) Predicted postoperative forced expiratory volume in one second (FEV1) of 800 ml
- (D) Residual volume to total lung capacity (RV/TLC) ratio of 0.35
- (E) Vital capacity of 3 liters
Which of the following is a cardiorespiratory effect of epidural block to a T4 sensory level?
- (A) Decreased expiratory reserve volume
- (B) Decreased tidal volume
- (C) Increased circulating catecholamine concentrations
- (D) Increased heart rate
- (E) Unchanged vital capacity
A 55-year-old woman who is scheduled to undergo carotid endarterectomy has a history of essential hypertension and chronic obstructive pulmonary disease. Over a 30-minute period beginning one hour after induction of general anesthesia, Sp02 decreases from 99% to 95%. During that time, she has received fentanyl 100 mcg, isoflurane 1%, nitrous oxide 49.5%, oxygen 49.5%, and a nitroglycerin infusion to maintain blood pressure at approximately 160/95 mmHg. Which of the following is the most likely cause for the decline in oxygen saturation?
- (A) Decreased cardiac output
- (B) Increased dead space ventilation
- (C) Inhibition of hypoxic pulmonary vasoconstriction
- (D) Mainstem intubation
- (E) Second gas effect
Preoperative evaluation of a patient who has marked malnutrition will demonstrate each of the following EXCEPT
- (A) decreased respiratory muscle function
- (B) decreased serum albumin concentration
- (C) decreased metabolic rate
- (D) suppressed immune function
- (E) decreased extracellular fluid volume
Two days after total abdominal hysterectomy, a 54-year-old woman develops lethargy followed by seizures and coma. Laboratory studies show a serum sodium concentration of 108 mEq/L and serum osmolality of 225 mOsm/kg. The most appropriate next step in management is administration of which of the following?
- (A) Desmopressin
- (B) Furosemide only
- (C) Saline solution 0.9% only
- (D) Furosemide and saline solution 0.9%
- (E) Furosemide and saline solution 3%
A 70-kg, 77-year-old man Is undergoing left nephrectomy with nitrous oxide, oxygen, fentanyl, and midazolam anesthesia. He has a 90 pack-year history of cigarette smoking and has chronic obstructive pulmonary disease. One hour after incision, expiratory wheezing occurs and peak Inspiratory pressure increases from 35 to 65 cmH20; end-tidal PCO2 is unchanged, but SpO2 decreases from 97% to 88%. The most likely cause is
- (A) endobronchial intubation
- (B) overinflation of the endotracheal tube cuff
- (C) pneumothorax
- (D) pulmonary edema
- (E) pulmonary embolism
During craniotomy in the sitting position, end-tidal carbon dioxide tension suddenly decreases. Ventilatory excursion of the chest is normal. Further evaluation is most likely to show a decrease in
- (A) alveolar-to-arterial oxygen tension difference
- (B) alveolar-to-arterial carbon dioxide tension difference
- (C) dead space ventilation
- (D) pulmonary artery pressure
- (E) pulmonary artery occlusion pressure
A patient undergoes thoracotomy in the lateral decubitus position. Which of the following maneuvers is most likely to increase PaO2 during one-lung ventilation?
- (A) Applying continuous positive airway pressure to the nondependent lung
- (B) Applying positive end-expiratory pressure to the dependent lung
- (C) Increasing inspiratory flow rate
- (D) Increasing the tidal volume
- (E) Increasing the ventilatory rate
A 29-year-old man who has been nasotracheally intubated for two weeks following a motor vehicle accident has a fever (39C) and a constant headache. Leukocyte count is 18,000/mm3. The most likely cause is
- (A) fractured nasal septum
- (B) retropharyngeal abscess
- (C) maxillary sinusitis
- (D) meningitis
- (E) rhinovirus infection
A pulmonary artery catheter is placed in an awake patient breathing room air. Typical right ventricular and pulmonary artery pressure tracings are obtained. With the catheter balloon inflated, blood drawn from the distal port has a PaO2 of 100 mmHg, while a simultaneous radial artery sample has a PaO2 of 90 mmHg. These data indicate that the
- (A) shunt fraction is greater than 10%
- (B) catheter is in the wedged position
- (C) catheter has entered a pulmonary vein
- (D) cardiac output is abnormally high
- (E) oxygen electrode is malfunctioning
In a patient with adult respiratory distress syndrome who is being mechanically ventilated, which of the following findings indicates the most severe disease?
- (A) Decreased functional residual capacity
- (B) Decreased lung compliance
- (C) Hypercarbia
- (D) Hypoxemia
- (E) Increased dead space
Which of the following statements about pulmonary function testing is true?
- (A) Forced expiratory volume in one second (FEV1) is directly related to maximum voluntary ventilation
- (B) FEV, is the most reliable indicator of small airways resistance
- (C) Forced vital capacity is markedly decreased in obstructive lung disease with air-trapping
- (D) Maximum mid-expiratory flow is less effort dependent than FEV1
- (E) Three-second forced expiratory volume is the amount of air exhaled during the third second of exhalation
Following pneumonectomy, a paralyzed patient being mechanically ventilated has the following arterial blood gas values: PaO2 71 mmHg, PaCO2 55 mmHg, pH 7.29. SvO2 is 45%. The most likely explanation for this SvO2 is
- (A) decreased red cell mass
- (B) high cardiac output
- (C) hypothermia
- (D) peripheral left-to-right arteriovenous shunt
- (E) ventilation / perfusion mismatch
Which of the following findings differentiates the pickwickian syndrome from morbid obesity?
- (A) Carbon dioxide retention
- (B) Upper airway obstruction
- (C) Decreased forced expiratory volume
- (D) Increased shunt fraction
- (E) Increased functional residual capacity
A 14-year-old girl with status asthmaticus is receiving oxygen 3 L/min through nasal prongs. Heart rate is 110 bpm. Arterial blood gas values are PaO2 90 mmHg, PaCO2 32 mmHg, and pH 7.46. If ventilation appears unchanged, which of the following is the most reliable sign of impending respiratory failure?
- (A) PaO2 of 80 mmHg
- (B) PaCO2 of 39 mmHg
- (C) Heart rate of 140 bpm
- (D) Increased wheezing
- (E) Deterioration of mental status
Which of the following statements concerning carbon monoxide poisoning is true?
- (A) Diagnosis is excluded if the PaO2 is greater than 300 mmHg while breathing 100% oxygen
- (B) Increased inspired oxygen concentration accelerates displacement of carbon monoxide from hemoglobin
- (C) Methylene blue decreases binding of carbon monoxide to hemoglobin
- (D) Pulse oximetry accurately reflects hemoglobin oxygen saturation
- (E) Tissue oxygen delivery is normal
If a patient with chronic obstructive pulmonary disease is uncooperative during pulmonary function testing, the most accurate assessment of his disease will be derived from the
- (A) forced expiratory volume in 1 second
- (B) forced midexpiratory flow
- (C) forced vital capacity
- (D) maximal voluntary ventilation
- (E) peak flow rate
The adult oxyhemoglobin dissociation curve will resemble that of the fetus in the presence of
- (A) increased 2,3-diphosphoglycerate concentration
- (B) chronic anemia
- (C) hyperthermia
- (D) metabolic alkalemia
- (E) hyperkalemia
A 35-kg child requires mechanical ventilation with 100% oxygen at a tidal volume of 350 mL and a rate of 20/min during a severe asthma attack. The most likely cause of severe hypotension after initiating mechanical ventilation is
- (A) hypoxic circulatory depression
- (B) inadequate expiratory time
- (C) increased pulmonary vascular resistance
- (D) respiratory alkalosis
- (E) tension pneumothorax
A 75-kg, 45-year-old patient with quadriplegia at the level of C6 is scheduled for elective cholecystectomy. Pulmonary function tests show an FVC of 2.4 L and an FEV, of 1.2 L. Which of the following is the most appropriate conclusion based on these findings?
- (A) Intercostal muscle function is normal
- (B) SpO, will be 80% or less while breathing room air
- (C) Total lung capacity is normal
- (D) The patient has chronic obstructive pulmonary disease
- (E) These findings are expected in this patient
A 56-year-old woman with pulmonary fibrosis is scheduled for pneumonectomy. Which of the following parameters best predicts potential postoperative functional impairment?
- (A) Exercise tolerance
- (B) Flow-volume loop
- (C) Resting arterial blood gas values
- (D) Unilateral pulmonary artery occlusion pressure
- (E) Vital capacity and FEV,
Which of the following changes in pulmonary function best explains the more rapid rate of rise of alveolar concentration of volatile anesthetics in pregnant women than in nonpregnant women?
- (A) Decreased functional residual capacity
- (B) Decreased dead space ventilation
- (C) Increased cardiac output
- (D) Increased oxygen consumption
- (E) Increased pulmonary venous admixture
Following a right lower lobectomy, a patient develops a bronchopleural fistula and becomes hypoxic. He is orally intubated and mechanically ventilated with pure oxygen. PaO2 is 65 mmHg, PaCO2 is 70 mmHg, and pH is 7.25. Which of the following will produce the most favorable change in the blood gases?
- (A) Increasing ventilatory frequency
- (B) Increasing suction on the chest tube
- (C) Applying 10 cmH2O positive end-expiratory pressure
- (D) Using a double-lumen tube for differential ventilation
- (E) Starting negative-pressure ventilation
Which of the following provides the most definitive diagnosis in a patient with suspected brain death?
- (A) Absent bilateral somatosensory evoked potentials
- (B) Absent cerebral blood flow during four-vessel contrast cerebral arteriography
- (C) Intracranial pressure greater than mean arterial pressure
- (D) Score of zero on Glasgow Coma Scale
- (E) Two isoelectric electroencephalograms
Peak airway pressure increases from 25 to 50 cmH2O when beginning right endobronchial ventilation with a right double-lumen tube. The most likely explanation for this increase is
- (A) failure to decrease tidal volume
- (B) inadvertent intubation of the left mainstem bronchus
- (C) intrinsic resistance of small endobronchial lumina
- (D) obstruction of the orifice of the right upper lobe
- (E) overinflation of the bronchial tube cuff
The sudden onset of pulmonary edema can be caused by each of the following EXCEPT
- (A) rapid re-expansion of the lungs following pneumothorax
- (B) upper airway obstruction
- (C) oxygen toxicity
- (D) rupture of mitral papillary muscle
- (E) severe preeclampsia
During one-lung ventilation, each of the following affects hypoxic pulmonary vasoconstriction in the nonventilated lung EXCEPT
- (A) application of continuous positive airway pressure to the nonventilated lung
- (B) high alveolar pO2 in the ventilated lung
- (C) infusion of isoproterenol
- (D) low mixed venous pO2
- (E) pulmonary hypertension
A 70-kg 22-year-old patient with head trauma and multiple fractures of the long bones is scheduled for fixation of bilateral femoral fractures. Preoperative laboratory studies show a serum sodium concentration of 150 mEq/L, a serum potassium concentration of 3.1 mEq/L, and a urine output greater than 500 ml/hr. Which of the following agents will decrease urine output?
- (A) 3% Saline solution
- (B) 5% Dextrose solution
- (C) Glucagon
- (D) Hydrocortisone
- (E) Vasopressin
Which of the following is the most likely beneficial effect of hyperbaric oxygen therapy in a 24-year-old scuba diver with decompression sickness?
- (A) Decreased production of carbon dioxide
- (B) Decreased size of gas bubbles
- (C) Increased functional residual capacity
- (D) Reversal of membrane pressure effects
- (E) Shift of the oxyhemoglobin dissociation curve to the left
A 50-year-old woman develops stridor 10 hours after undergoing thyroidectomy. The most appropriate management is administration of which of the following drugs?
- (A) Albuterol
- (B) Calcium chloride
- (C) Ipratropium bromide
- (D) Racemic epinephrine
- (E) Triiodothyronine
During right upper lobectomy and one-lung ventilation with a double-lumen endotracheal tube, the PaO2 decreases to 40 mmHg. The PaCO2 is 39 mmHg. Which of the following is most appropriate?
- (A) Confirm position of the tube with bronchoscopy
- (B) Apply 5 cmH20 continuous positive airway pressure to the nondependent lung
- (C) Apply 5 cmH20 positive end-expiratory pressure to the dependent lung
- (D) Resume two-lung ventilation
- (E) Clamp the pulmonary artery of the nondependent lung
Which of the following statements concerning pulmonary function in patients with pulmonary fibrosis is true?
- (A) Diffusion capacity is decreased
- (B) Pulmonary artery diastolic-to-occlusion pressure gradients are normal
- (C) Ventilation-perfusion relationships are normal
- (D) Static pulmonary compliance is unchanged
- (E) Mechanical ventilation with slow rate and large tidal volume is optimal
The acute onset of hypotension without a decrease in mixed venous oxygen saturation is most likely associated with the onset of
- (A) hemorrhage
- (B) myocardial infarction
- (C) pulmonary edema
- (D) pulmonary embolus
- (E) sepsis
A 1-month-old infant becomes hypoxemic faster during apnea than an adult. Which of the following is the primary cause of this difference?
- (A) Functional residual capacity in an infant is half that of an adult
- (B) Metabolic rate in an infant is twice that of an adult
- (C) Resting PaO2 in an infant is lower than that in an adult
- (D) The number of alveoli in an infant is 12% the number in an adult
- (E) The hemoglobin dissociation curve in an infant is shifted to the right
Two days after myocardial infarction involving the left anterior descending coronary artery, a patient's blood pressure decreases acutely from 125/80 to 70/40 mmHg, heart rate increases from 75 to 90 bpm, pulmonary artery pressure increases to 50/30 mmHg, and urine output decreases from 60 to 10 ml/hr. Thermodilution cardiac output has increased from 4 to 7 L/min. The most appropriate action is to
- (A) compare mixed venous oxygen saturation in the right atrium and pulmonary artery
- (B) draw blood for culture and start antibiotic therapy
- (C) start dopamine infusion in low dose
- (D) administer a fluid challenge
- (E) monitor peripheral capillary oxygenation by transcutaneous oximetry
You are called to a witnessed cardiac arrest where cardiopulmonary resuscitation is being performed. After successful intubation, arterial blood gas values are PaO2 86 mmHg, PaCO2 63 mmHg, and pH 7.25 at an FiO2 of 1.0. The most appropriate management at this time is to
- (A) repeat arterial blood gas analysis using a new specimen
- (B) administer sodium bicarbonate
- (C) administer fluid challenge with 500 ml of normal saline solution
- (D) hyperventilate the patient
- (E) add positive end-expiratory pressure
A 90-kg, 59-year-old man with chronic obstructive pulmonary disease is undergoing laparotomy. Mechanical ventilation is being carried out with a fresh gas flow of 2 L/min at a rate of 16/min and tidal volume of 900 ml; I:E ratio is 1:2.5. PaCO2 remains greater than 50 mmHg. Preoperative PaCO2, was normal. Which of the following is the most appropriate next step?
- (A) Adding 10 cmH20 of positive end-expiratory pressure
- (B) Converting to spontaneous ventilation
- (C) Decreasing inspiratory flow rate
- (D) Increasing exhalation time
- (E) Increasing fresh gas flow
A 60-kg, 17-year-old girl with severe idiopathic scoliosis is scheduled for Harrington rod fixation. Which of the following respiratory parameters is compatible with this disorder?
- (A) Alveolar-to-arterial oxygen tension difference (A-aDO2) less than 100 mmHg while breathing pure oxygen
- (B) FEV1/FVC ratio less than 50%
- (C) Forced vital capacity less than 2000 ml
- (D) Intrapulmonary shunt less than 10%
- (E) Normal pulmonary vascular resistance
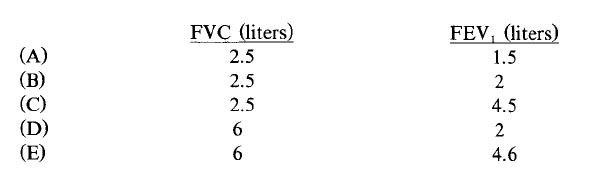
A 57-year-old man who weighs 150 kg and is 170 cm (67 in) tall is scheduled for cholecystectomy. He has a 100 pack-year smoking history. Which of the following findings on pulmonary function testing are most likely?
At extubation performed one week after nasotracheal intubation, each of the following is likely to occur EXCEPT
- (A) upper airway obstruction
- (B) aspiration after extubation
- (C) ulceration of vocal cords
- (D) tracheal stenosis
- (E) sinusitis
A patient is scheduled for right pneumonectomy. A left-sided double-lumen endobronchial tube is inserted. After the endobronchial side is clamped and both cuffs are inflated, breath sounds are heard only on the left. Which of the following is the most likely cause?
- (A) Herniation of the endobronchial cuff over the carina
- (B) Occlusion of the right upper lobe bronchus
- (C) Placement of the endobronchial lumen in the left mainstem bronchus
- (D) Placement of the endobronchial lumen in the right mainstem bronchus
- (E) Placement of the endobronchial lumen in the trachea
A 120-kg 56-year-old man undergoing gastrectomy during anesthesia with fentanyl and isoflurane has a PetCO2 of 35 mmHg and a PaCO2 of 50 mmHg. His FEV,/FVC ratio is 80% of predicted. Heart rate is 120 bpm and arterial blood pressure is 80/40 mmHg. Which of the following is the most likely cause of the difference in PaCO2 and PetCO2?
- (A) Aspiration pneumonitis
- (B) Chronic obstructive pulmonary disease
- (C) Decreased cardiac output
- (D) Decreased VD/VT ratio
- (E) Increased QS/QT ratio