10 Random Questions
Compared with the response of a normal patient, administration of a bolus dose of pancuronium (0.15 mg/kg) to a patient with cirrhosis and ascites would be associated with
- (A) longer duration
- (B) more rapid onset
- (C) more intense block
- (D) more difficult reversibility
- (E) similar pharmacokinetics
A 54-year-old woman who is scheduled to undergo emergency exploratory laparotomy takes warfarin sodium for anticoagulation. Prothrombin time is 19 sec (control 12 sec). Which of the following agents is most appropriate to reverse the effects of warfarin?
- (A) Cryoprecipitate
- (B) Desmopressin (DDAVP)
- (C) Factor IX concentrate
- (D) Fresh frozen plasma
- (E) Pooled factor VIII
Phantom limb pain is an example of which of the following types of pain?
- (A) Central pain
- (B) Nociceptive pain
- (C) Psychosomatic pain
- (D) Sympathetically mediated pain
- (E) Vasospastic pain
A 45-kg, 80-year-old woman undergoes pin fixation of the right hip in the lateral decubitus position under spinal anesthesia. One day after the operation, she cannot move her left ankle or foot actively. The most likely cause is
- (A) compression of the sciatic nerve
- (B) compression of the common peroneal nerve
- (C) injury of the nerve root at L4-5
- (D) stretching of the femoral nerve
- (E) stretching of the tibial nerve
Which of the following statements concerning the innervation of the larynx is true?
- (A) The glossopharyngeal nerve provides motor innervation to the vocal cords
- (B) The recurrent laryngeal nerve provides sensory innervation to the mucosa of the larynx above the vocal cords
- (C) The hypoglossal nerve provides sensory innervation to the aryepiglottic folds
- (D) Unilateral recurrent laryngeal nerve injury results in an abducted vocal cord on the injured side
- (E) The vagus nerve provides innervation to all structures below the vocal cords
Which of the following findings best indicates complete resolution of spinal anesthesia?
- (A) Ability to ambulate
- (B) Ability to urinate
- (C) Perianal pinprick sensation
- (D) Pain at the surgical site
- (E) Proprioception of the big toe
A 2.3-kg 1-day-old term infant requires repair of a gastroschisis. Which of the following combinations is most appropriate for intraoperative fluid management?
- (A) Dextrose 5% in water for maintenance and lactated Ringer's solution for replacement of third space losses
- (B) Dextrose 10% in water for maintenance and lactated Ringer's solution for replacement of third space losses
- (C) Lactated Ringer's solution for maintenance and replacement of third space losses
- (D) Lactated Ringer's solution for maintenance and albumin 5% for replacement of third space losses
- (E) Normal saline solution for maintenance and lactated Ringer's solution for replacement of third space losses
Each of the following decreases hepatic blood flow EXCEPT
- (A) isoflurane anesthesia
- (B) spinal anesthesia
- (C) hypercarbia
- (D) mechanical ventilation
- (E) positive end-expiratory pressure
The preanesthetic ECG trace (lead II) shown from a 32-year-old woman suggests
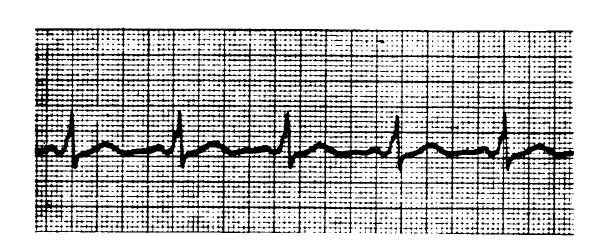
- (A) potential for tachyarrhythmia
- (B) need for preanesthetic atropine
- (C) myocardial ischemia
- (D) left bundle branch block
- (E) right ventricular hypertrophy
Each of the following values is associated with acute tubular necrosis EXCEPT
- (A) urine osmolality of 200 mOsm/kg
- (B) urine sodium concentration of 15 mEq/L
- (C) urine specific gravity of 1.009
- (D) urine/serum osmolarity ratio of 1.2
- (E) fractional excretion of sodium of 4%